
Article
Integrating Nutritional Assessment into Geriatric Pet Care: A Clinical Framework for Vets
Aging in dogs and cats brings progressive changes in metabolism, digestion, and body composition that directly influence health, longevity, and quality of life. Detecting nutritional issues early is central to preventive veterinary care.
Veterinarians play a pivotal role in assessing whether an animal’s current diet supports its physiological needs and in identifying when nutritional intervention or adjustment is required. A systematic nutritional evaluation conducted alongside standard clinical examination enables early detection of malnutrition, obesity, or subclinical disease linked to dietary imbalance.
Nutritional Assessment: The Fifth Vital Sign
The World Small Animal Veterinary Association (WSAVA) recognizes nutritional assessment as the fifth vital sign, emphasizing its inclusion in every routine consultation.
Even without specialist nutrition training, veterinarians can implement a structured first-line evaluation to answer one key question:
Does this pet medically require a change in nutrition or dietary prescription?
This approach can be performed independently in general practice, supported by digital tools, or in collaboration with a veterinary nutritionist for complex cases1.
Step 1: Diet Assessment
A thorough understanding of the pet’s current feeding pattern is the cornerstone of nutritional evaluation. The veterinarian should record all food sources—commercial diets, home-prepared meals, treats, supplements, and table scraps—ideally maintained consistently for at least one month.
During the owner interview, four practical questions help collect reliable data2:
- What food do you give to your pet?
- What else, and in what amount daily?
- Are you satisfied with your pet’s current diet?
- What changes would you like to make?
These simple questions establish the foundation for identifying nutritional risk factors.
Table 1. Interpreting Diet Type and Risk1,2,3
|
Diet Category |
Description |
Clinical Note |
|
Diet (1): Balanced commercial food |
Complete and species-appropriate, with treats ≤10% of caloric intake |
Usually acceptable if health and condition are stable |
|
Diet (2): Non-targeted or risk-prone diet |
Includes homemade, raw, vegan, or mixed diets, or excessive treats |
May predispose to nutritional imbalances or contamination risks |
Clinical interpretation:
This table helps differentiate between diets that are nutritionally complete and appropriate versus those that pose potential risks. Diet (2) scenarios often require correction, especially in older pets with lower metabolic tolerance.
Step 2: Pet Assessment
After evaluating the diet, the next step is to assess the pet’s clinical and physical condition. Subtle changes in body or coat condition often signal nutritional inadequacy before biochemical abnormalities appear.
Table 2. Physical Indicators of Nutritional Status2
|
Parameter |
Optimal Findings |
Requires Action If |
|
Body weight & condition |
Ideal weight and BCS |
Underweight or overweight |
|
Muscle condition |
Normal tone and symmetry |
Muscle loss, especially temporal/lumbar |
|
Coat & skin |
Glossy coat, healthy skin |
Dull coat, dandruff, erythema, alopecia |
|
Dental health |
Clean teeth, pink gums |
Gingivitis, tartar, or oral inflammation |
|
Digestive health |
Firm stools, 1–3/day |
Vomiting, diarrhea, flatulence, constipation |
|
Urinary health |
Normal urine output and pH |
Abnormal pH (<6 or >7), crystals, blood |
|
New disease |
None |
Any metabolic/systemic condition affecting diet |
Clinical interpretation:
This checklist serves as a quick visual reference during physical exams. Recording each parameter allows veterinarians to identify whether dietary modification may improve or stabilize the pet’s condition—particularly relevant in geriatrics where subtle deficits have outsized clinical effects.
Step 3: Integrating Findings into Clinical Action
Integrating dietary data with clinical findings allows veterinarians to prioritize interventions and decide whether a change is preventive or therapeutic.
Table 3. Clinical Decision Matrix2
|
Assessment Combination |
Recommended Clinical Action |
|
Diet (1) + Pet (A) |
No change needed; re-evaluate at next check-up or upon condition change |
|
Diet (2) + Pet (A) |
Adjust to a balanced, age-appropriate diet with correct nutrient proportions |
|
Diet (1) + Pet (B) |
Review feeding quantity, nutrient density, and specific needs; modify accordingly |
|
Diet (2) + Pet (B) |
Full dietary correction required; consider referral to a veterinary nutritionist |
Clinical interpretation:
This matrix translates assessment findings into clear action steps. For example, even pets on balanced diets (Diet 1) may show poor condition (Pet B) due to incorrect feeding amounts or comorbidities. It ensures that every nutrition-related decision is evidence-guided rather than assumption-based.
Step 4: Monitoring and Follow-Up
Following any dietary change, monitoring is essential to confirm compliance, assess tolerance, and detect early deviations2.
- Pets should be re-evaluated approximately one month after initiating a new diet.
- In cats, intermediate checks are advisable due to their sensitivity to food transitions.
- Monitoring should include a repeat nutritional assessment, adjustment of diet quantity or type if required, and evaluation of clinical response.
Follow-up frequency should reflect the animal’s health status and life stage. At every subsequent visit, nutritional assessment—recognized by WSAVA as a vital sign—should be included in the routine examination.
Any unexpected change (weight, appetite, stool, coat quality) warrants investigation. When clinical targets (e.g., ideal body weight) are achieved, the dietary plan should be revised to maintain long-term stability.
Conclusion
In aging dogs and cats, nutritional assessment is not an adjunct—it is a core element of preventive medicine.
By systematically integrating diet evaluation, physical assessment, and structured follow-up into every consultation, veterinarians can detect and correct nutritional imbalances early.
Routine, evidence-based monitoring ensures that each animal’s dietary plan continues to meet its evolving physiological needs—supporting healthier, longer lives.
References
- Villaverde C, Chandler M. Commercial vs homemade cat diets: what you need to know. J Feline Med Surg 2022;24(5):415–428.
- Blanchard G, Priymenko N, Oh WS. Nutrition and aging in dogs and cats: assessment and dietary strategies. Journal of Veterinary Science. 2025 Sep 24;26(Suppl 1):S96.
- Choi B, Kim S, Jang G. Nutritional evaluation of new alternative types of dog foods including raw and cooked homemade-style diets. Journal of Veterinary Science. 2023 Aug 7;24(5): e63.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
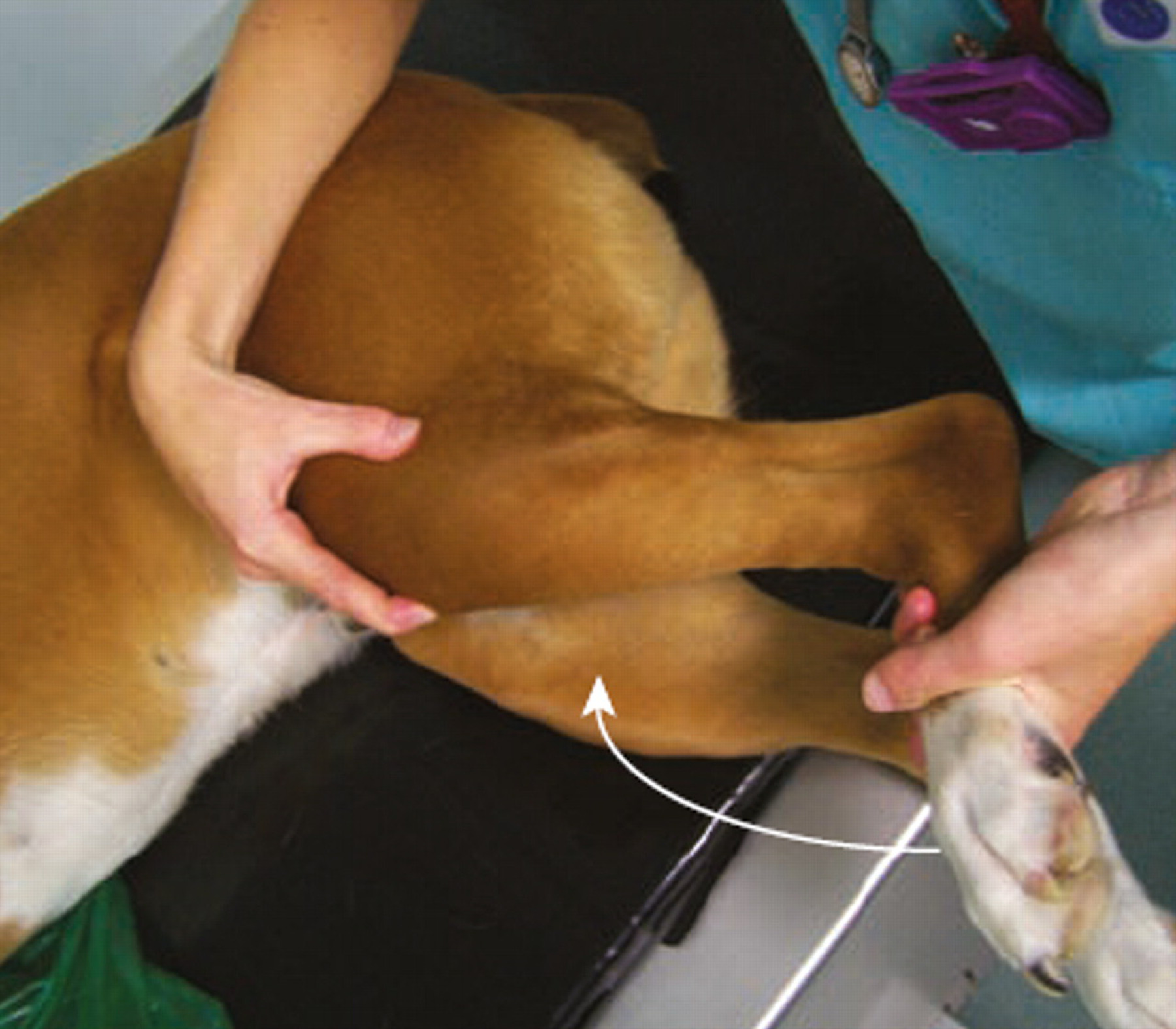
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...