
Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be intricately linked rather than separate domains. Modern health challenges, such as emerging infectious diseases, antimicrobial resistance, food safety risks, and environmental degradation, cannot be fully addressed by any single sector acting alone. Instead, a One Health approach emphasizes interdependence among these fields and promotes collaboration to protect the health of all life forms and ecosystems. One Health seeks to “sustainably balance and optimize the health of people, animals and ecosystems,” recognizing that these systems operate together, not in isolation.
The Interconnected Web of Health
Environmental conditions strongly influence disease dynamics in humans and animals. Ecosystem disruptions caused by deforestation, climate change, and pollution alter habitats and species interactions, creating opportunities for pathogen emergence. Changes in land use and climate affect vector habitats and increase contact between humans and wildlife, thereby influencing the patterns and risks of zoonotic diseases, as emphasized within the One Health framework supported by the World Health Organization1.
Why this matters1:
- Environmental degradation can increase pathogen survival in soil and water.
- Climate shifts can expand the geographic range of disease vectors like mosquitoes.
- Pollution and habitat loss undermine the natural barriers between wildlife and human populations.
These ecological drivers create a shared risk environment where the health of ecosystems directly influences risks to animal and human populations.
Animal Health: A Bridge Between Environment and Humans
Animals, both domestic and wild, serve as sentinels and conduits for environmental and human health threats. Diseases that originate or circulate in animal populations often reflect underlying environmental pressures (e.g., water contamination, degraded habitats) and can later affect human health.
For example, studies show that livestock water sources become contaminated when environmental factors such as seasonal rainfall patterns and sewage discharge intersect with animal husbandry practices. The convergence of these environmental and animal health risk factors increases the likelihood of zoonotic pathogens entering human communities2.
This demonstrates that animal health cannot be separated from environmental context: ecological conditions shape pathogen transmission patterns, and animal infections often signal problems that also threaten human health.
Human Health and Environmental Drivers
Furthermore, some neglected tropical diseases, particularly soil-transmitted helminth infections, clearly demonstrate how environmental reservoirs of pathogens contribute to transmission between animals and humans. Contaminated soil and water act as persistent sources of infection, allowing parasites to circulate across human, animal, and environmental interfaces 3,4,5. Mathematical modeling studies that explicitly include environmental compartments show that soil and water reservoirs play a central role in maintaining transmission dynamics and infection persistence3.
These findings highlight that disease control strategies focused solely on human treatment are insufficient and underscore the need for integrated One Health approaches that simultaneously address environmental sanitation, animal health, and human health.
Bridging the Gaps Through One Health
Systematic reviews of One Health research indicate that, although the One Health concept is widely adopted, its practical implementation remains uneven. Analyses of published studies show that most One Health research primarily focuses on human and animal health interactions, while environmental health components are less consistently incorporated. As a result, environmental drivers of disease—such as ecosystem disruption, land use change, and environmental contamination—are often insufficiently examined alongside animal and human health outcomes6.
These findings highlight a structural gap within One Health research frameworks. Without adequate integration of environmental data, the interconnected pathways linking ecosystems, animals, and humans cannot be fully understood. Reviews emphasize that this imbalance limits the ability of One Health approaches to explain disease emergence and persistence in complex socio-ecological systems.
To address this limitation, the literature stresses the importance of stronger interdisciplinary collaboration. Effective One Health practice requires coordinated efforts among veterinary professionals, public health experts, environmental scientists, and policy stakeholders. Such collaboration supports integrated surveillance, shared data systems, and preventive strategies that account for environmental conditions alongside animal and human health factors. Strengthening this integration is essential for translating One Health from a conceptual framework into a functional, evidence-based approach for disease prevention and health protection 6.
Conclusion: A Unified Vision for Health
Addressing global health challenges requires recognizing that environmental health, animal health, and human health are deeply intertwined. Environmental changes shape the health of animals, and both influence human well-being. A One Health framework, supported by integrated research and practical action, offers a holistic pathway to confront complex health threats such as zoonotic diseases, antimicrobial resistance, and environmental degradation.
By breaking down traditional silos and fostering transdisciplinary collaboration, we can better anticipate, prevent, and respond to health risks that span ecosystems, animal populations, and human communities.
References
- Humboldt-Dachroeden S, Mantovani A. Assessing environmental factors within the one health approach. Medicina. 2021 Mar 5;57(3):240.
- Yenew C, Temesgen A, Gebeyehu AA, Enawgaw AS, Yemata GA, Ejigu AG, et al. One Health-related risk factors and seasonal variations in zoonotic bacteriological contamination of livestock water sources. Sci Rep. 2025;15:44464. doi:10.1038/s41598-025-28199-9.
- Okongo W, Muhumuza C, Aguegboh NS, Bwambale E, Diallo B. Mathematical modelling of the co-infection dynamics of soil-transmitted helminths and schistosomiasis with optimal control. Boundary Value Problems. 2025 Dec;2025(1):1-38.
- Chan AH, Pakdee W, Kaenkaew C, Sungpradit S, Charoennitiwat V, Kusolsuk T, Thaenkham U. One Health implications and first evidence of environmental contamination of helminths in soil from goat farms in Ratchaburi, Thailand. Parasitology Research. 2025 Aug;124(8):89.
- Cuevas AJ, Aguilar KK, Monserrat EA, Padayao JC, Servigon MM, Turingan AM, Dorado BB, Ignacio JM, Lodor PF, Osete AN, Ramo AF. One health investigation of enteric parasites at the human–animal–soil interface in a marginalized peri-urban Philippine community. Discover Public Health. 2025 Dec;22(1):760.
- Kuhn C, Hayibor KM, Acheampong AT, Pires LS, Costa-Ribeiro MC, Burrone MS, Vásquez-Almazán CR, Radon K, Soto MT, Salini AP, Marcia A. How studies on zoonotic risks in wildlife implement the one health approach–A systematic review. One Health. 2024 Dec 1;19:100929.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
.jpg)
Article
Concurrent Endocrine Disorders in Canine Diabetes: Diagnostic and Therapeutic Implications for Clinical Practice
In dogs with diabetes mellitus, persistent hyperglycaemia or wide glycaemic vari...
Article
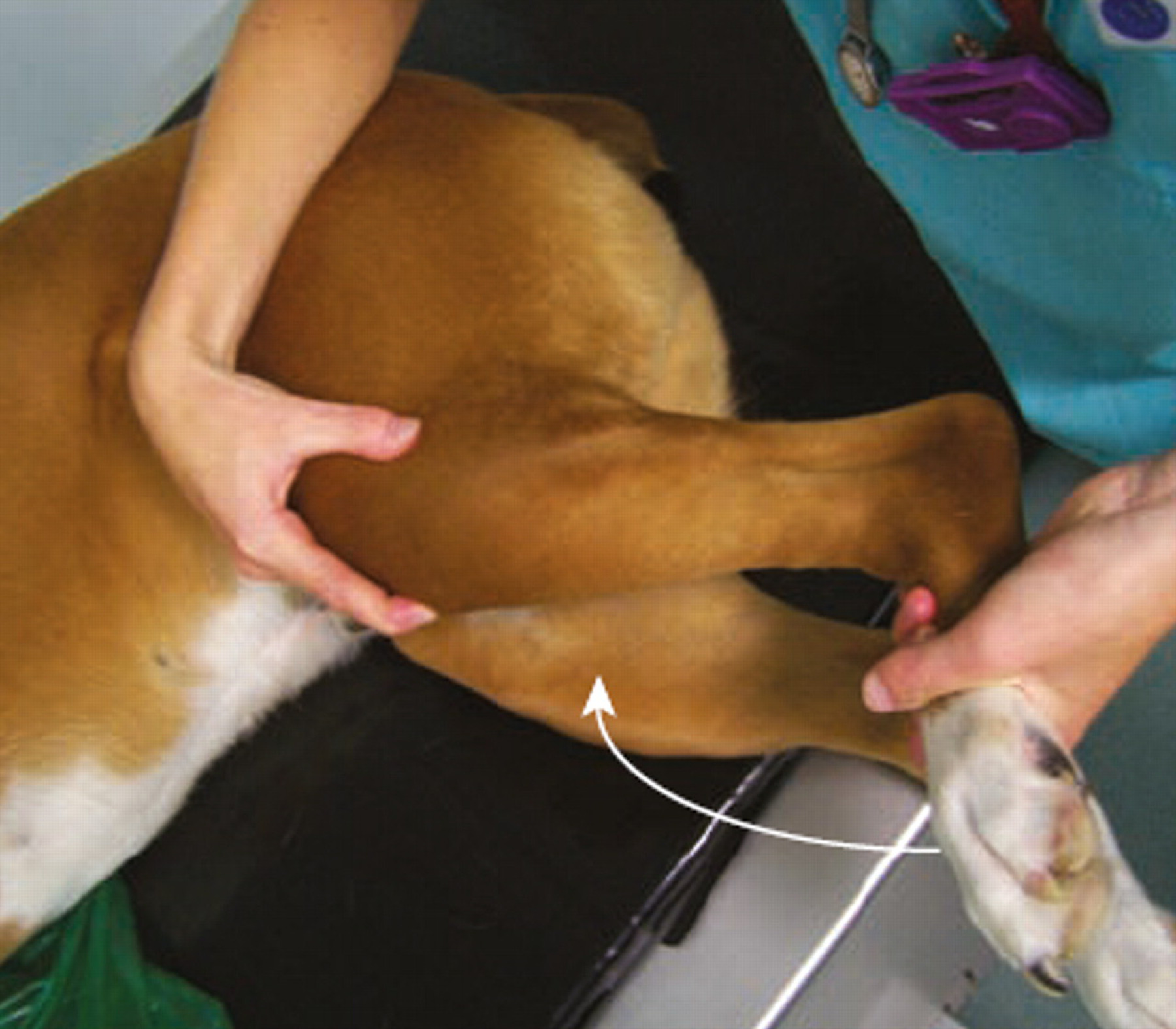
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...