
Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, animals, and the environment. Resistant pathogens compromise the effectiveness of antibiotics and other antimicrobial agents, threatening routine medical treatment, disease control, and veterinary care alike. Addressing AMR effectively requires integrated, cross-sectoral collaboration that moves beyond traditional professional boundaries. AMR’s drivers include the misuse of antimicrobials in both human and animal medicine, environmental contamination, and lack of coordinated surveillance systems1,2.
The One Health Imperative
The One Health approach recognizes that the health of humans, animals, and ecosystems is interdependent. Integrated strategies in research, surveillance, and clinical practice can yield more effective AMR mitigation than siloed efforts. The One Health framework is crucial because resistant microorganisms and resistance genes circulate across species and environments, driven by interconnected use of antimicrobials in livestock, companion animals, and humans1.
Integrated Surveillance and Data Linkage
Current Surveillance Limitations
A comprehensive scoping review of integrated surveillance systems found that although there is strong theoretical support for integrated antibiotic resistance surveillance, actual operationalized systems are limited. Most existing models do not fully span human, animal, and environmental domains, and standardized protocols are lacking1.
Another systematic review underscored a key gap: data on antimicrobial use, resistance prevalence, stewardship activities, and infection control are typically analyzed in isolation. Linking disparate AMR datasets can reveal previously unseen trends and improve the evidence base for coordinated intervention strategies across health sectors 2.
Surveillance and Veterinary Medicine
For veterinary professionals, surveillance must include animal pathogens and antimicrobial usage data from agricultural and clinical settings. Integration of these animal sector data with human and environmental surveillance improves understanding of transmission pathways, especially those that cross species barriers.
Systems Thinking and Regional Approaches
A regional One Health study applied systems thinking to map AMR interactions. It emphasized the importance of involving stakeholders from the earliest stages of strategic planning, including veterinary professionals, policymakers, environmental managers, and human health experts. Systems thinking enables a fuller understanding of causal relationships and shared leverage points within AMR dynamics, crucial for coordinated regional action3.
In veterinary contexts, systems thinking highlights how animal health practices (such as antibiotic use in livestock and companion animals) can influence resistance patterns in human and environmental microbes.
Genomics and Emerging Technologies
Technological tools such as whole-genome sequencing (WGS), metagenomics, and advanced bioinformatics are transforming AMR surveillance. Genomic approaches allow high-resolution tracking of resistance genes and transmission patterns across species, providing insights not achievable with conventional methods. These tools support source attribution and help identify emerging resistance before clinical failure occurs4.
For veterinary laboratories, incorporating genomic surveillance enhances diagnostics and strengthens capacity to detect and monitor resistance trends relevant to animal health and zoonotic transmission.
Challenges in Integrating AMR Strategies
Despite recognition of One Health benefits, integration faces several barriers:
- Fragmented Governance: Inconsistent policies across human, animal, and environmental sectors impede unified action1.
- Data Silos: Separate data repositories in human health, veterinary medicine, and environmental monitoring reduce interoperability.
- Resource Disparities: Low-resource settings often lack laboratory infrastructure and trained personnel for comprehensive surveillance1.
Veterinary professionals should advocate for cross-disciplinary data sharing and co-designed surveillance frameworks that respect the unique contributions and constraints of animal health settings.
Communication and Stewardship Integration
Effective AMR communication requires engagement of veterinarians alongside clinicians and public health professionals. Public and professional education on responsible antimicrobial use in both human and animal sectors supports stewardship goals and reduces unnecessary prescriptions.
Stewardship programs must be implemented in veterinary clinics and farms to promote evidence-based antibiotic use and reduce selective pressure for resistance. These programs benefit from shared strategies and benchmarks developed jointly by human and animal health professionals.
Conclusion: Why Breaking Silos Matters to Veterinary Medicine
AMR is a shared problem that transcends professional domains. For veterinary professionals, the implications are twofold:
- Clinical Impact: Resistant infections complicate treatment in animals, with potential for zoonotic spillover.
- Collaborative Role: Participation in integrated surveillance, research, and stewardship is necessary for effective AMR control.
Veterinary expertise is essential in One Health initiatives, from contributing animal antimicrobial usage and pathogen data to co-leading stewardship and education efforts. Breaking professional silos strengthens the entire health ecosystem’s ability to respond to AMR.
References
- Delpy L, Astbury CC, Aenishaenslin C, Ruckert A, Penney TL, Wiktorowicz M, Ciss M, Benko R, Bordier M. Integrated surveillance systems for antibiotic resistance in a One Health context: a scoping review. BMC Public Health. 2024 Jun 27;24(1):1717.
- van Kessel SA, Wielders CC, Schoffelen AF, Verbon A. Enhancing antimicrobial resistance surveillance and research: a systematic scoping review on the possibilities, yield and methods of data linkage studies. Antimicrobial Resistance & Infection Control. 2025 Mar 29;14(1):25.
- Huebner C, Huebner NO, Goerig T, Flessa S. A regional One Health approach to mapping antimicrobial resistance interactions via systems thinking. One Health Outlook. 2025 Dec;7(1):1-8.
- Chigozie VU, Aniokete CU, Ogbonna PI, Iroha RI. Transforming antimicrobial resistance mitigation: the genomic revolution in one health and public health. Discover Applied Sciences. 2025 Oct 13;7(10):1187.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
.jpg)
Article
Concurrent Endocrine Disorders in Canine Diabetes: Diagnostic and Therapeutic Implications for Clinical Practice
In dogs with diabetes mellitus, persistent hyperglycaemia or wide glycaemic vari...
Article
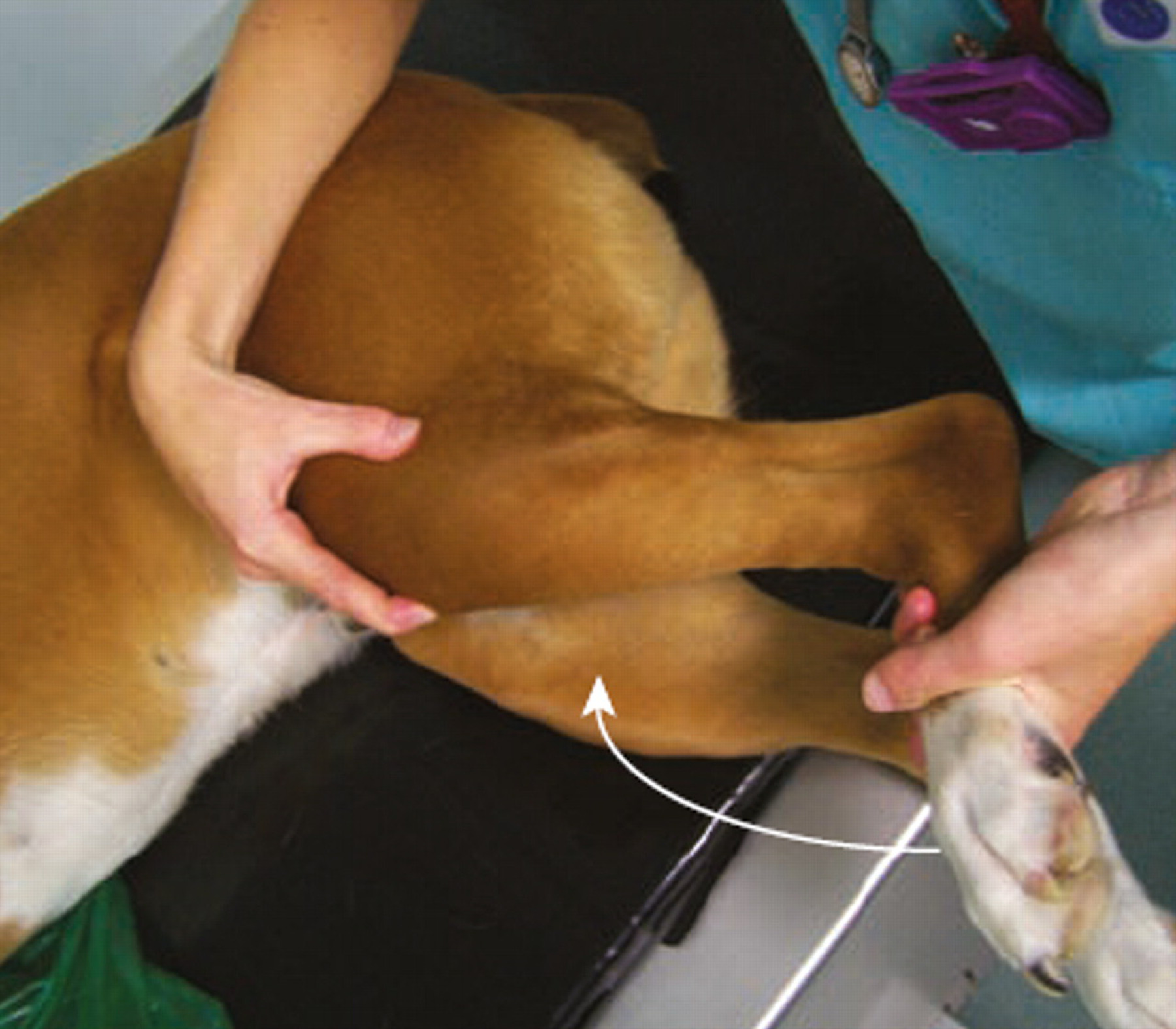
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...