
Article
Feline LUTD Management: Disease-Specific Guidelines for Veterinarians – iCatCare 2025
Introduction
Lower urinary tract signs (LUTS) in cats—such as dysuria, haematuria, pollakiuria, stranguria, and periuria—are common and potentially serious presentations. The 2025 iCatCare Guidelines provide a structured approach to managing LUTD, including Feline Idiopathic Cystitis (FIC), urolithiasis, urinary tract infection (UTI), and urethral obstruction (UO)1. Given overlapping clinical signs, a disease-specific management strategy is essential for improving patient outcomes and owner compliance.
1. Feline Idiopathic Cystitis (FIC)
Management
- Multimodal Environmental Modification (MEMO): Increase litter box number (one more than number of cats), ensure cleanliness, reduce stressors, and provide vertical and horizontal enrichment2.
- Hydration & diet: Aim for total water intake ≥ 25–30 mL/kg/day (food moisture + water) to reduce recurrence risk. Encourage wet-food diets (≥70% moisture) and multiple water sources1.
- Analgesics/adjuncts: Buprenorphine 0.01–0.02 mg/kg IV/SC/SL Q8–12h for acute episodes1
- Monitoring: Track recurrence of LUT signs and reassess MEMO compliance; studies report ~70–75% reduction in recurrence with consistent environmental management1.
2. Urolithiasis
Management by Stone Type
- Struvite stones: Consider medical dissolution using diet and optimize hydration3.
- Calcium oxalate stones: Surgical removal is usually necessary; post-operative prevention focuses on diet and hydration4.
Supportive Care
- Encourage hydration to maintain dilute urine (USG < 1.030 where possible)5
- Pain management: Opioids or NSAIDs if renal function permits1.
Follow-Up
- Recheck urinalysis and imaging every 6–12 months.
- Ensure ongoing access to fresh water and monitor diet compliance.
3. Urinary Tract Infection (UTI)
Management
- Confirm diagnosis via urine culture and sensitivity (cystocentesis sample preferred)1.
- Subclinical bacteriuria: Usually not treated; consider only in diabetics, suspected pyelonephritis, or pre-urinary surgery1,6.
- Clinical UTI: Treat based on culture & sensitivity; provide analgesia (NSAID or opioid).
- Empirical therapy: Amoxicillin or trimethoprim-sulfonamide; avoid cefovecin or fluoroquinolones unless resistant or severe cases1,6.
- Treatment duration1,6:
- Simple UTI: 3–5 days
- Complicated/recurrent: 7–14 days
- Pyelonephritis: longer as needed
- Resistance: Enterococcus spp. resistant to beta-lactams, cephalosporins, TMP-SMX, fluoroquinolones1.
- Adjunct/supportive care:
- Increase hydration and voiding frequency
- Reduce stress; provide environmental enrichment
- Analgesia if mobility issues limit urination7
Monitoring
- Re-culture after therapy in recurrent or complicated cases.
- Address underlying comorbidities to prevent recurrence.
4. Urethral Obstruction (UO)
Emergency Management
- Stabilization: Evaluate for hyperkalaemia and cardiovascular compromise.
- Calcium gluconate 10%: 0.5–1 mL/kg IV over 2–3 min if ECG abnormalities (peaked T-waves, bradycardia) are present1.
- Fluid therapy: Initial IV rate 10–20 mL/kg/hr until obstruction relieved; maintenance ~50 mL/kg/day (~2 mL/kg/hr).
- Decompression: Catheterization preferred; cystocentesis if catheterization delayed or unsafe1.
- Analgesia: Buprenorphine for 5–7 days post-obstruction.
Post-Obstruction & Monitoring
- Monitor urine output hourly; post-obstructive diuresis often > 2 mL/kg/hr.^6
- Adjust fluid therapy accordingly.
- Check serum electrolytes and PCV/TS every 8–12 hours until stable1.
Prevention of Recurrence
- Identify underlying cause (FIC, urolithiasis, UTI).
- Implement MEMO, hydration, and urinary diet plans post-discharge.
Key Takeaway
Effective management of feline lower urinary tract diseases requires a disease-specific approach, combining emergency stabilization, targeted pharmacologic therapy, supportive care, and environmental management. Feline idiopathic cystitis, urolithiasis, urinary tract infections, and urethral obstruction each demand tailored interventions based on clinical presentation, underlying cause, and comorbidities.
Key principles include:
- Prioritizing life-threatening emergencies (e.g., hyperkalaemia in urethral obstruction).
- Using culture-guided antimicrobial therapy for UTIs and avoiding unnecessary or empiric use of critically important antibiotics.
- Promoting hydration, stress reduction, and environmental enrichment across all LUTD types.
- Educating owners on recurrence prevention, dietary modification, and early recognition of signs.
By integrating these evidence-based strategies, veterinarians can improve clinical outcomes, reduce recurrence, and enhance quality of life for feline patients with LUTD.
References
- Taylor S, Boysen S, Buffington T, Chalhoub S, Defauw P, Delgado MM, Gunn-Moore D, Korman R. 2025 iCatCare consensus guidelines on the diagnosis and management of lower urinary tract diseases in cats. Journal of feline medicine and surgery. 2025 Feb;27(2):1098612X241309176.
- Kurum H, Yalcin E. Effects of multimodal environmental modification in crystal-related feline lower urinary tract diseases. Arquivo Brasileiro de Medicina Veterinária e Zootecnia. 2023 Jul 17;75:665-72.
- Westropp JL, Delgado M, Buffington CT. Chronic lower urinary tract signs in cats: current understanding of pathophysiology and management. Veterinary Clinics: Small Animal Practice. 2019 Mar 1;49(2):187-209.
- Buote NJ, Hayes G, Bisignano J, Rosselli D. Retrospective comparison of open vs minimally invasive cystotomy in 28 cats using a composite outcome score. Journal of Feline Medicine and Surgery. 2022 Oct;24(10):1032-8.
- Heseltine J. Diagnosing and Managing Feline Lower Urinary Tract. Texas A&M University College of Veterinary Medicine & Biomedical Sciences. 2019;45:1307-10.
- Weese JS, Blondeau J, Boothe D, Guardabassi LG, Gumley N, Papich M. ISCAID guidelines for the diagnosis and management of bacterial urinary tract infections in dogs and cats. The Veterinary Journal. 2019;241:8-25.
- Al-Anany AM, Hooey PB, Cook JD, Burrows LL, Martyniuk J, Hynes AP, German GJ. Phage therapy in the management of urinary tract infections: a comprehensive systematic review. Phage. 2023 Sep 1;4(3):112-27.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
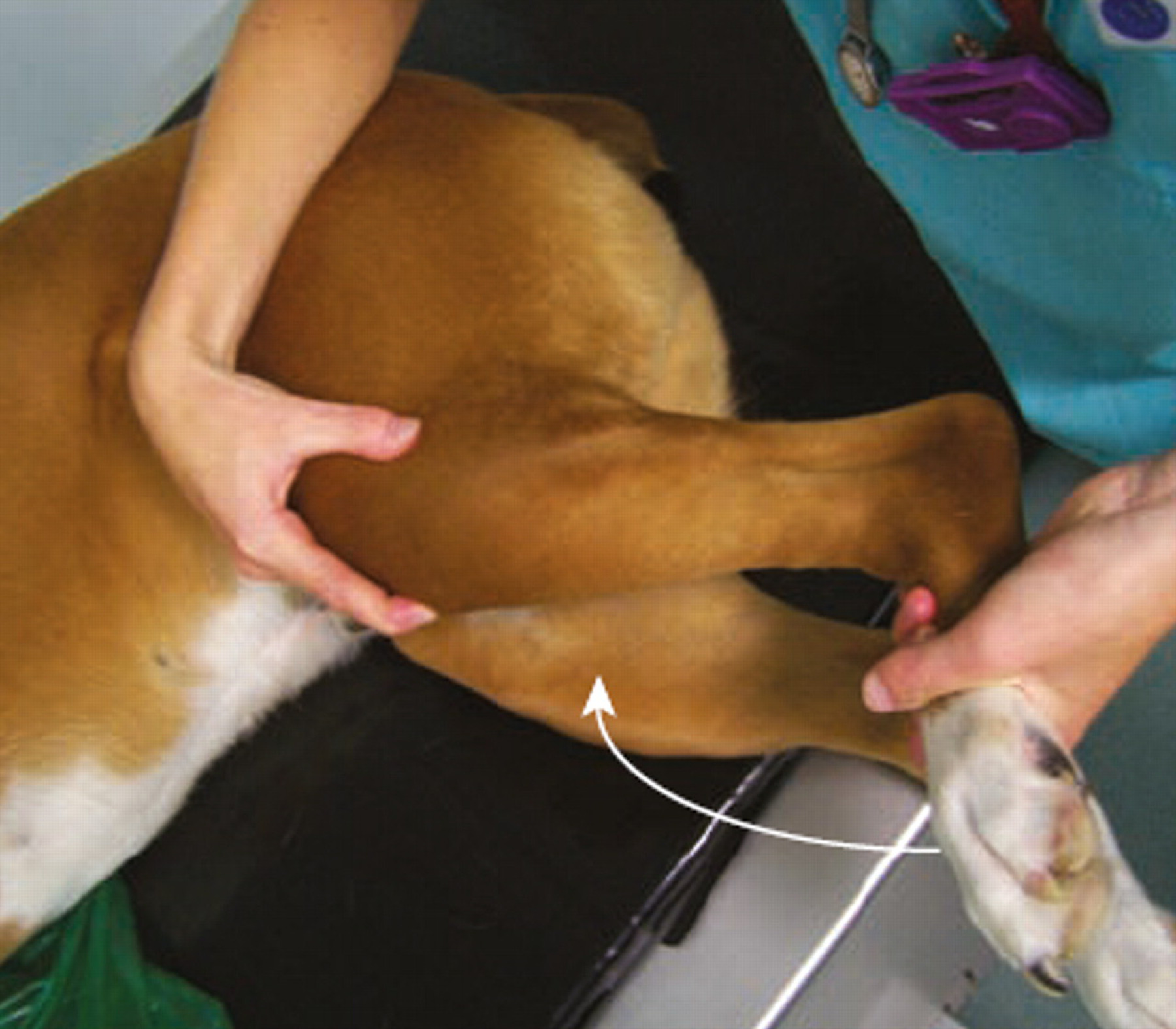
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...