
Article
Diagnosing MUO in Practice: MRI, CSF, and When to Biopsy
No fever, Bloodwork normal, but still, a small-breed dog is acting strangely, presenting with sudden seizures and circling. Now, you are standing at a clinical crossroads: is it Meningoencephalitis of unknown origin (MUO) or an infection you can’t afford to miss?
MUO is one of the most common causes of acute-onset brain disease in small-breed dogs. Ruling out MOU is easy, but confirming it without overlooking a treatable condition is a challenging task.
Let’s explore the stepwise diagnostic approach, which is smart, safe, and effective.
- Start with Suspicion: Identify the Red Flags
MOU can easily be mistaken for a seizure disorder or stroke. Breeds such as Pug, Maltese, and Yorkshire Terriers are mainly affected by MUO1.
Clinical signs reflect focal or multifocal CNS lesions.
- Common neurological signs include2:
- Seizures
- Ataxia
- Proprioceptive deficits
- Vestibular signs
- Blindness
- Multiple cranial nerve deficits
- Head or neck pain (occasionally)
- Systemic signs like fever are rare
- GME typically affects the forebrain, brainstem, or both
- GME can rarely present as meningomyelitis, causing:
- Paresis
- Spinal ataxia
- Spinal cord-only involvement in ~9.5%–13% of cases
- MRI: The First Line of Insight
MRI is the most crucial step in diagnosing MOU. MRI findings include asymmetrical, multifocal T2 hyperintensities located in the forebrain or cerebellum 3.
It’s important to look for2
- GME: Periventricular or cerebellar white matter lesions
- NME: Gray matter necrosis (Pugs, Maltese)
- NLE: Bilateral white matter damage (Yorkies)
Pro Tip: Always include contrast-enhanced T1-weighted sequences in the MRI protocol to visualize a mild, focal, unilateral temporal muscle lesion 4.
Mistake to Avoid: Don’t rely solely on MRI for diagnosis—MUO can mimic other CNS diseases radiographically5
- CSF Analysis: Timing is everything
Cerebrospinal Fluid (CSF) helps to identify inflammatory changes and rule out infections. CSF key findings include elevated protein and predominantly mononuclear pleocytosis 2.
Key points to keep in Mind
- Always image before CSF tap to rule out herniation risk.
- Avoid sampling if MRI shows mass effect or midline shift.
- Use sterile handling — contamination ruins PCR reliability.
Pro Tip: If MRI suggests MUO but CSF is bland, repeat after 48–72 hours inflammation may not yet have peaked.
Mistake to Avoid: Avoid starting corticosteroids before CSF collection — even one dose can suppress cytology and delay diagnosis.
- Excluding Infectious Encephalitis: Don’t Skip the Rule-Outs
Before labeling a case as MUO, it’s essential to rule out infectious causes such as canine distemper virus, toxoplasmosis, neosporosis, and ehrlichiosis. These pathogens can mimic MUO both clinically and radiographically.
Recommended approach:
- Run PCR and/or serology on both blood and CSF
- Perform testing before initiating corticosteroids, which may suppress pathogen detection and skew results
Pro Tip: A negative PCR doesn’t confirm absence — it only means the pathogen wasn’t detectable in that sample.
Mistake to Avoid: Don’t assume every negative test confirms MUO. False negatives can occur due to timing, sample quality, or intermittent shedding. Always interpret results in context with imaging and CSF findings.
- Biopsy: The Diagnostic Decider
Histopathology is necessary to confirm the disease. Without such a diagnostic tool, MUO remains a presumptive diagnosis2.
Indications for biopsy:
- Atypical MRI (single lesion, ring enhancement)
- Poor response to immunosuppression
- Large-breed dogs (MUO less likely)
Pro Tip: A targeted stereotactic biopsy gives both diagnosis and direction. It’s not a last resort; it’s a clarifier.
Mistake to Avoid: Delaying biopsy following extended steroid administration may compromise histologic interpretation.
- Putting It All Together: The Smart Diagnostic Workflow
- Signalment + Neuro Exam → suspect MUO
- MRI → map lesion pattern
- CSF tap → confirm inflammation
- PCR/Serology → rule out infection
- Biopsy (if ambiguous or poor response)
Final Takeaway
While MUO can appear complex, a structured approach makes the difference. Recognize the pattern, get MRI promptly, perform CSF analysis carefully, and reserve biopsy for unclear cases. Early immune diagnosis can be the deciding factor in recovery.
Related Experts
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
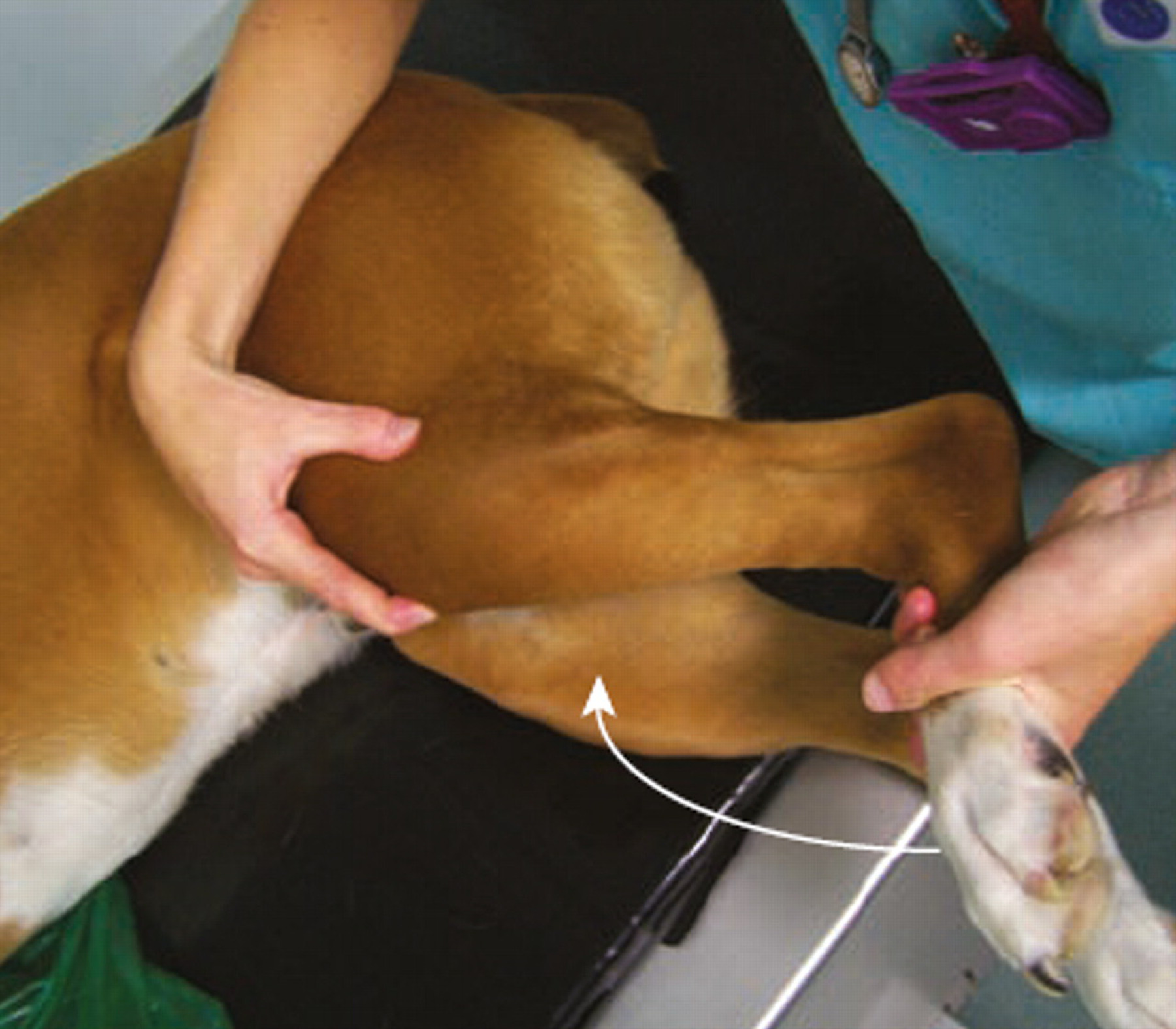
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...
