
Article
Feline OA is Real - How to Diagnose It Without Radiographs
Feline osteoarthritis (OA) is a widely under-recognized condition in clinical practice, particularly in India, where awareness about chronic pain in cats remains limited.
Epidemiological studies suggest that up to 61% of cats over the age of six show radiographic signs of OA, with the number rising significantly in cats over 12 years (Lascelles et al., 2012). However, due to the subtlety of feline behaviour and their evolutionary predisposition to mask pain, clinical detection is challenging.
Unlike dogs, cats with OA do not often exhibit overt lameness. Instead, veterinarians should look for reduced grooming, difficulty jumping onto furniture, reluctance to use the litter box, irritability, or social withdrawal. A validated owner questionnaire such as the Feline Musculoskeletal Pain Index (FMPI) or Client Specific Outcome Measures (CSOM) can
provide valuable insight into mobility changes that may not be obvious during examination (Benito et al., 2013).
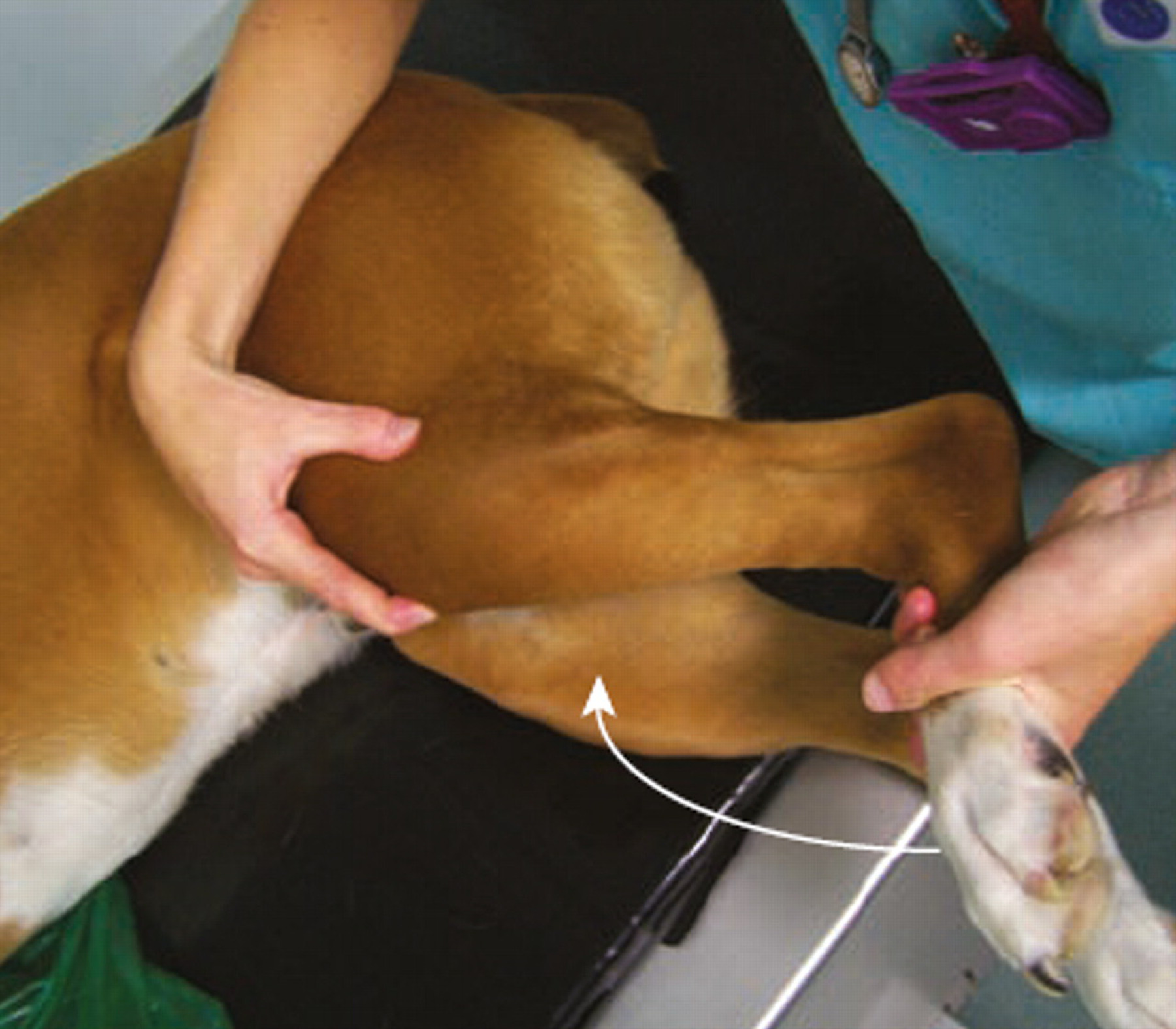
Orthopaedic examination in cats can be complicated by their temperament, but careful palpation of the spine, hips, elbows, and stifles may reveal crepitus, joint thickening, or reduced range of motion. Radiographs can confirm OA but often underestimate the pain burden; cats with mild radiographic changes may have significant functional impairment.
Management of feline OA should focus on pain control and environmental adaptation. Pharmacological options include meloxicam (off-label, at the lowest effective dose) and gabapentin, which provides analgesia and anxiolysis during handling. Non-drug approaches
include padded bedding, easy-access litter trays, warm resting spots, and ramps to reduce jumping. Newer therapies such as frunevetmab, a feline anti-NGF monoclonal antibody, show promise in clinical trials (Enomoto et al., 2022), though availability in India is still emerging.
Early recognition and a multimodal management strategy can greatly improve quality of life. Veterinary practitioners in India should prioritize feline OA in senior wellness exams, and educate guardians about behavioural pain signs.
References:
- Lascelles BDX et al. (2012). https://pubmed.ncbi.nlm.nih.gov/20561321
- Benito J et al. (2013). https://pubmed.ncbi.nlm.nih.gov/23369382
- Enomoto M et al. (2022). https://pubmed.ncbi.nlm.nih.gov/30368458
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...