
Article
Ulcer or Not? — A Practical, Evidence-Based Approach to Corneal Ulcers
Corneal ulceration remains one of the most time-critical presentations in small-animal and equine ophthalmology. Despite its frequency, early assessment is often deceptively challenging: subtle surface changes can mask significant stromal compromise, while intense blepharospasm or tearing may occur even when the epithelium is intact. For clinicians in general practice, this makes the initial question — “ulcer or not?” — a decisive moment that shapes the entire diagnostic and therapeutic pathway.
The consequences of misclassification are well documented: delayed recognition of complicated ulcers increases the risk of infection, stromal melting, perforation, and vision loss; whereas unnecessary aggressive treatment of a non-ulcerative condition can worsen inflammation or delay healing.
The first 30 seconds: rapid triage
When a patient presents with a red, painful eye: start with basic observation (blepharospasm, epiphora, eyelid conformation), then perform a fluorescein stain immediately. Because intact corneal epithelium resists fluorescein uptake (lipophilic), while exposed stroma binds the hydrophilic dye, any stromal uptake reliably indicates a breakdown of the epithelium — i.e., a true ulcer1.
This is supported by recent work advocating regular fluorescein application, even for home-based monitoring of superficial ulcers2.
After staining, examine the size, shape, edge definition, stromal opacity, and presence of any infiltrate or discharge. A small, well-demarcated, non-infected superficial ulcer behaves very differently from a large, irregular, undermined defect with grey-white stromal opacity or “soft” melting edges.
2. Immediate on-site management: act fast, but thoughtfully
Uncomplicated superficial ulcers
Bacterial infection is common in canine stromal corneal ulcers, with Staphylococcus pseudintermedius, S. epidermidis, S. capitis, and Pseudomonas aeruginosa being the most frequently isolated pathogens3.
Empiric therapy with a broad-spectrum topical antibiotic alone typically covers the majority of isolates. For broader coverage, combination therapy with fluoroquinolone or aminoglycoside may be used until culture and susceptibility results are available3 .
Clinical Note: Initiate empiric therapy promptly to control infection but adjust treatment based on culture and sensitivity to ensure effectiveness and limit resistance.
3. Sampling: cytology & culture — don’t delay
For all deep, melting, or non-improving ulcers, perform cytology (scrape/impression) and bacterial ± fungal culture. Early sampling guides therapy identifies resistant organisms or fungal pathogens and avoids blind or ineffective treatment4.
While cytology alone may detect bacteria or fungi, culture directs targeted therapy, allowing de-escalation and reducing drug toxicity.
4. Anti-protease / anti-collagenase therapy for melting ulcers
When keratomalacia (stromal melting) is evident, anticollagenase therapy is indicated:
Topical autologous serum or plasma rich in α₂-macroglobulin and protease inhibitors, slows stromal collagen breakdown1.
Topical chelating agents, e.g., EDTA, bind zinc and calcium, cofactors for matrix metalloproteinases5.
Systemic doxycycline may be considered for its MMP-inhibitory effect in selected cases1.
Recent reports suggest that early application of these measures can stabilize melting ulcers even before culture results return6.
5. When to refer for surgery or graft-based repair
If the ulcer progresses to descemetocele, perforation, or fails to respond to aggressive medical therapy, refer promptly. Options include conjunctival flaps, corneal grafts (buccal mucosa, amniotic membrane, PRF membrane), or temporary tissue adhesives1,6.
Studies show autologous buccal mucosa grafts restore globe integrity in most deep/perforated ulcers. PRF membrane grafts are emerging as effective adjuncts in deep canine ulcers when specialist surgery is delayed6.
6. Species- and setting-specific considerations
Dogs (brachycephalic breeds): Predisposed to exposure keratopathy and self-trauma; eyelid/conformation correction plus ulcer therapy prevents recurrence3.
Horses / large animals: High risk of fungal keratitis (plant trauma); early cytology, culture, antifungal therapy, and referral are critical4.
Resource-limited settings: Intensive medical therapy may salvage superficial and early stromal ulcers, but prognosis is guarded without surgical support6.
Conclusion
First, fluorescein remains the single most valuable diagnostic tool. Then stratify quickly: superficial ulcers respond well to conservative therapy, while deep or melting ulcers demand aggressive management, early sampling, and close rechecks. Preventing proteolysis is critical, as anticollagenase therapy significantly improves the chances of preserving the globe. Refer promptly when indicated; descemetoceles, perforations, and non-responsive deep ulcers warrant timely surgical intervention⁶. And always tailor decisions to the species, breed predispositions, and the practical realities of each clinical setting.
References
- Farghali HA, Abouelnasr KS, Nasr EA, Elsherif A. Corneal ulcer in dogs and cats: novel clinical application of regenerative therapy using subconjunctival injection of autologous platelet-rich plasma. Front Vet Sci. 2021;8:616164.
- Li Puma MCL, Valli A, Dore M, et al. A remote fluorescein staining and photography protocol for monitoring of ulcerative keratitis in small animal patients. Vet Ophthalmol. 2023;26:85–92.
- Joksimovic M, Trbolova A, Brkljacic M, et al. Antibiotic recommendations for treatment of canine stromal corneal ulcers. Vet Sci. 2023;10(2):66.
- Tahoun A, Abd-Elhafeez HH, El-Shafaey EA, et al. Epidemiological and molecular investigation of ocular fungal infection in equine from Egypt. Vet Sci. 2020;7(3):130.
- MSD Veterinary Manual. Anti-inflammatory and antiproteolytic agents in animals.
- Kumar ASK, Rameshkumar K, Selvaraj P, et al. Management of deep corneal ulcer in a dog using autologous platelet-rich fibrin (PRF) membrane. J Vet Anim Sci. 2024.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
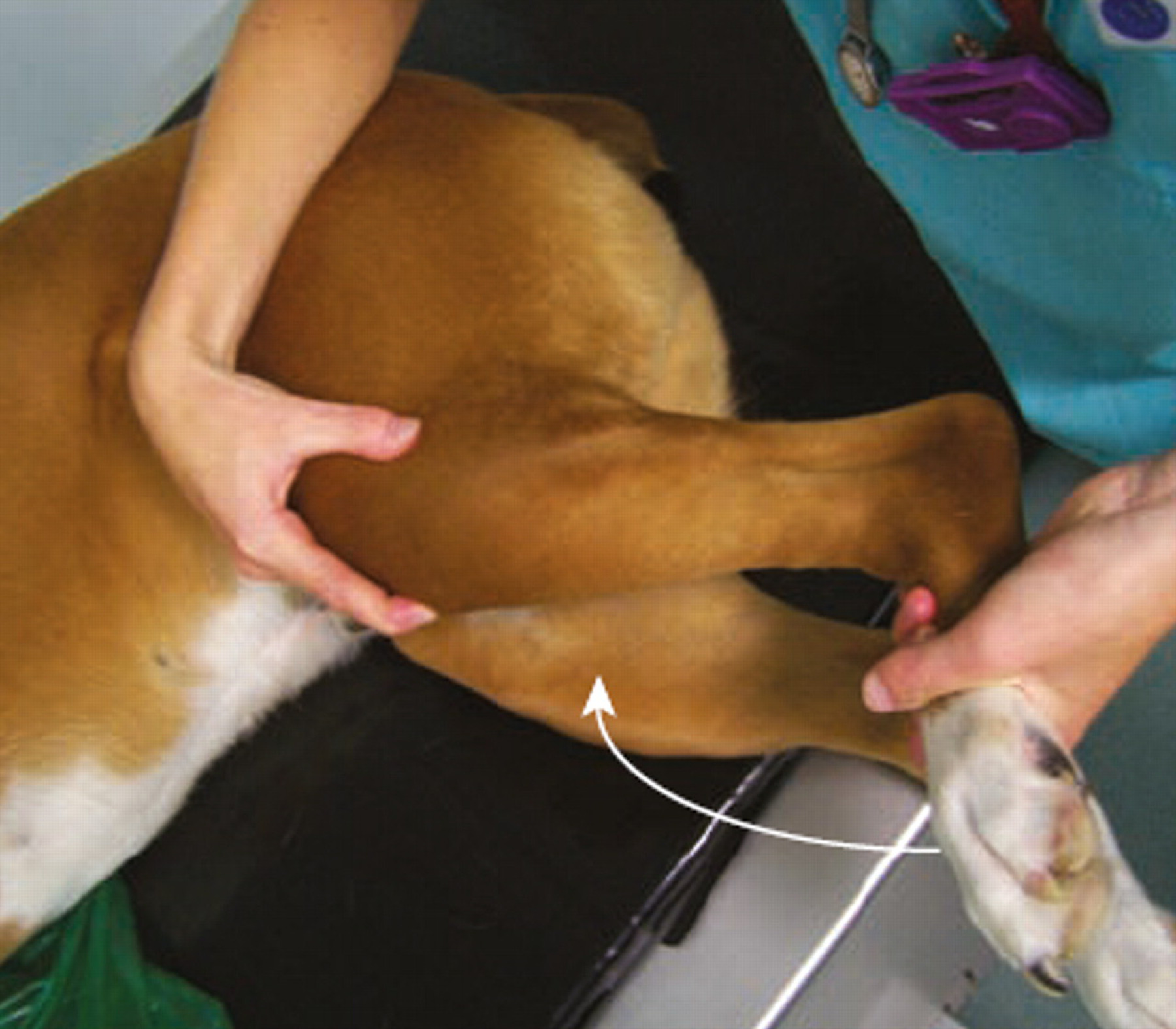
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...