
Article
Fixed-Rate Insulin CRI in Decompensated Diabetic Dogs: A Practical Guide for Veterinarians
Introduction
Diabetic dogs presenting in decompensated states whether diabetic ketoacidosis (DKA) or severe hyperglycemia with dehydration require rapid, controlled medical stabilization. A standardized low-dose insulin continuous-rate infusion (CRI) provides predictable glucose-lowering, reduces metabolic fluctuations, and minimizes the risk of iatrogenic hypoglycemia. Several studies have shown that dogs treated with low-dose CRI protocols achieve meaningful glycemic reductions within clinically appropriate timeframes, with consistent safety across a range of disease severities1.
But in a busy emergency setting, can one simplified insulin protocol reliably stabilize dogs across such a wide spectrum of diabetic crises?
Recent clinical evaluations using a fixed-rate infusion (FRI) of regular insulin at 0.05 IU/kg/h demonstrated that dogs experience a rapid glucose decline during the first hours of therapy, followed by stabilization around the 6-hour mark2,3. This pattern was observed in dogs with severe hyperglycemia, dehydration, and early-stage DKA, defined as mild-to-moderate ketosis without marked acidosis (venous pH > 7.25) 3. The early, controlled reduction in glycemia, often >50% within 6 hours highlights the effectiveness of a simple standardized approach2.
Why Choose a Fixed-Rate Low-Dose CRI?
Low-dose regular insulin CRI (0.05–0.1 U/kg/hr) maintains a steady plasma insulin concentration, promoting gradual glucose decline and steady ketone suppression4. This consistency prevents abrupt osmotic changes and reduces electrolyte derangements that commonly complicate DKA management.
FRI protocols are preferred in many emergency settings because they:
- Simplify calculations
- Reduce dosing errors
- Provide more predictable results than intermittent SC/IM dosing
- Allow stable, continuous suppression of ketogenesis
Prospective research by Gant et al. (2020) supports the use of fixed low-dose CRI as an effective and safe strategy1.
FRI vs. VRI: Which Is Better in Practice?
Both fixed-rate infusion (FRI) and variable-rate infusion (VRI) are used in veterinary emergency medicine, each with distinct advantages:
Fixed-Rate Infusion (FRI)
0.05 IU/kg/h constant rate
- Easier to standardize
- Lower risk of calculation errors
- Predictable glycemic decline
- Less intensive mathematical monitoring
- Comparable outcomes to VRI in ketone clearance1,2
Variable-Rate Infusion (VRI)
Dose adjusted in real time based on BG
- Allows personalized dosing
- Ideal when close monitoring staff is available
- Higher workload
- Increased chance of miscalculation, especially in busy hospitals2
Recent comparative data suggest similar clinical outcomes, but shorter hospitalization and fewer adjustments with FRI1. For most general and emergency practices, a standardized FRI protocol offers a safer, more practical approach.
When to Start a Fixed-Rate CRI
Initiate FRI when dogs present with:
- BG > 300–350 mg/dL
- Clinical dehydration
- Hyperosmolar state
- Any degree of ketosis or ketoacidosis
- Persistent vomiting or inability to take SC insulin
- Neurologic signs associated with hyperglycemia
Start CRI after 1–2 hours of isotonic crystalloid resuscitation.
Recommended CRI Protocol
Insulin
- Regular insulin at 0.05–0.1 U/kg/hr
- Prime the line with insulin-containing fluid to saturate binding sites2
Fluids
- Use isotonic crystalloids
- Add dextrose once BG reaches 200–250 mg/dL to prevent hypoglycemia and allow continued ketone clearance
Monitoring
- BG: every 1–2 hours
- Electrolytes (K⁺, P): every 4–6 hours
- Venous blood gas: to track acidosis
- Ketones: blood or urine every 6–8 hours
Expected Clinical Response
Dogs typically demonstrate a 50–100 mg/dL/hour glucose decline in the first several hours2,3. Glycemic stabilization often appears by hour 6, with ketosis and acid–base status improving over the next 12–24 hours2. This timeline helps predict treatment response and identify non-responders early.
When to Transition Off CRI
Switch to SC insulin when the dog:
- Is rehydrated
- Is eating voluntarily
- Has BG < 250 mg/dL with declining ketones
- Shows improving acid–base balance
Give the first SC dose 1–2 hours before discontinuing CRI to avoid rebound hyperglycemia.
Common Pitfalls and How to Avoid Them1,2
- Overly Rapid BG Drop (>100 mg/dL/hr)
→ Reduce CRI by 25–50% or increase dextrose.
- Persistent Hyperglycemia
→ Re-prime the line, check pump accuracy, confirm catheter patency.
- Electrolyte Crashes (K⁺, P)
→ Supplement early; do not wait for severe deficits.
Practical Veterinary Pearls2
- Prime Smart: Discard 20–30 mL after adding insulin to the line.
- Fluids First: Poor perfusion delays glycemic response.
- Ketones Lag Behind: Continue insulin with dextrose even after BG normalizes.
- Assume K⁺ Will Fall: Start supplementation early.
- Always Aim for Gradual Decline: 50–100 mg/dL/hr prevents neurologic complications.
Conclusion
A standardized low-dose fixed-rate insulin CRI is an effective, practical, and safe method for stabilizing decompensated diabetic dogs. When paired with robust monitoring and proactive electrolyte support, FRI provides predictable glycemic control and reduces complications. Its simplicity, reproducibility, and evidence-supported outcomes make it a strong first-line protocol for most veterinary emergency settings.
References
- Gant P, Barfield D, Florey J. Comparison of insulin infusion protocols for management of canine and feline diabetic ketoacidosis. Journal of Veterinary Emergency and Critical Care. 2024 Jan;34(1):23-30.
- González F, Díaz F, Pereira I, Siel D. Efficacy of a Standardized Low-Dose Insulin Infusion Protocol in the Emergency Stabilization of Diabetic Dogs. Veterinary Sciences. 2025 Oct;12(10):968.
- Wildermuth, D.; Chew, D.J.; DiBartola, S.P.; Schenck, P.A.; Brown, S.A. The use of a fixed low-dose insulin CRI protocol in emergency diabetic management. Vet. Med. Today 2021, 20, 89–96.
- Fleeman L, Gilor C. Insulin therapy in small animals, part 1: general principles. Veterinary Clinics: Small Animal Practice. 2023 May 1;53(3):615-33.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
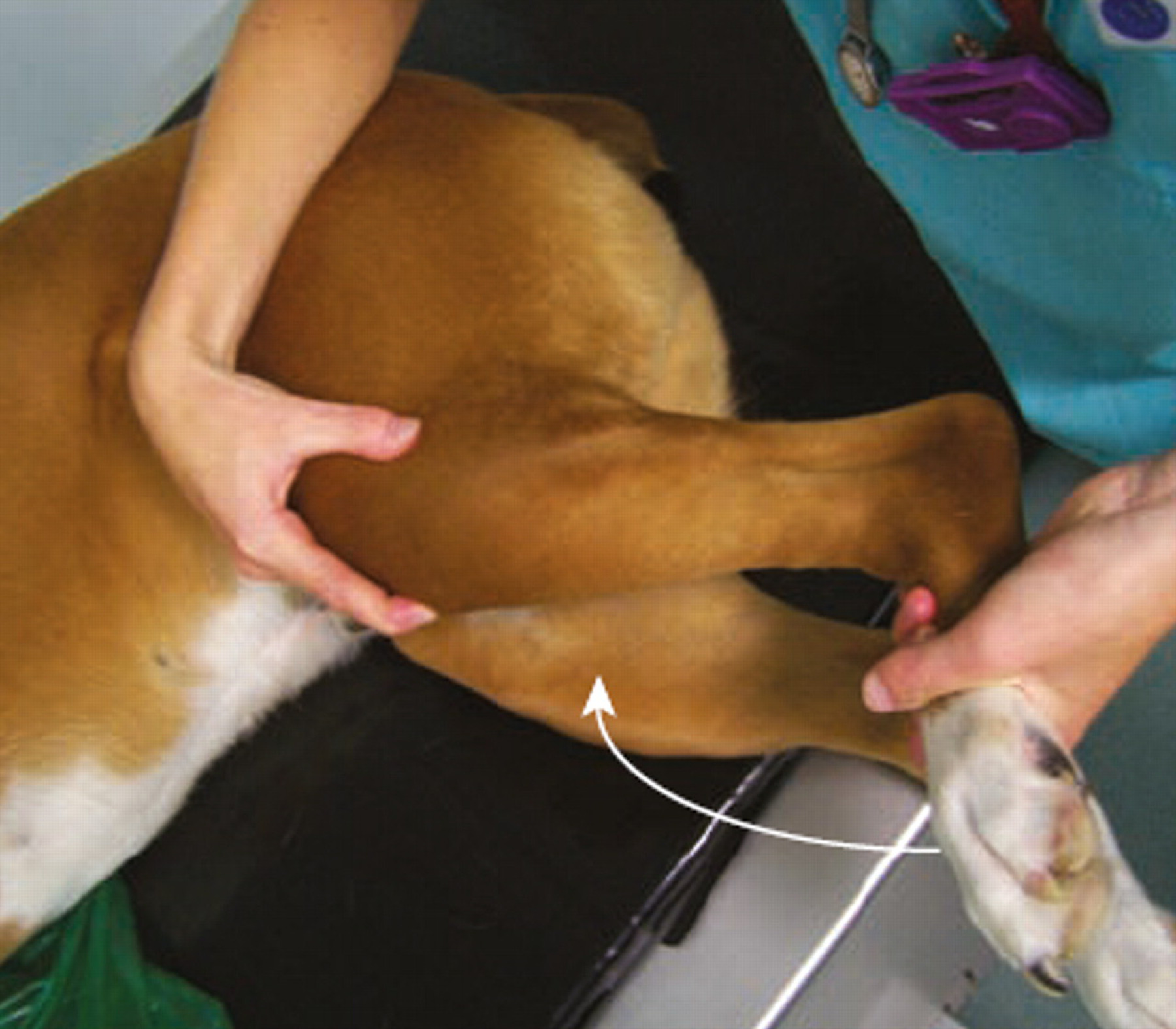
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...