
Article
Diabetes Mellitus in Dogs: A Clinical Update for Practitioners
Diabetes mellitus (DM) in dogs remains one of the most frequently diagnosed endocrine disorders in small-animal practice. While typically seen in middle-aged to older dogs, juvenile diabetes—though rare—poses unique diagnostic and management challenges. A recent report by Daravigka et al. (2025) highlights such a scenario, describing a five-month-old female dog with juvenile diabetes mellitus complicated by a pancreatic abscess, successfully managed through ultrasound-guided drainage and medical therapy1.
Clinical presentation and diagnosis
The young dog presented with polyuria, polydipsia, vomiting, and poor growth. Physical examination revealed cachexia (BCS 1.5/5), dehydration, and weak peripheral pulses. Laboratory findings were consistent with diabetic ketoacidosis:
- Fasting hyperglycemia (≈ 406 mg/dL)
- Elevated fructosamine (336 µmol/L) and HbA1c (4.3%)
- Marked ketonemia (β-hydroxybutyrate = 5.9 mmol/L)
- Glycosuria and ketonuria
Despite the metabolic crisis, pancreatic lipase (cPL) and trypsin-like immunoreactivity (cTLI) were normal, suggesting no overt pancreatitis or exocrine insufficiency.
Abdominal ultrasound revealed a thick-walled cystic lesion (~2 × 1.2 × 1 cm) within the pancreatic body. Cytology confirmed pyogranulomatous inflammation, consistent with a pancreatic abscess, although culture was sterile.
Pathophysiological insights
Pancreatic abscesses are uncommon in dogs and typically arise from necrotizing pancreatitis or infection of pre-existing pseudocysts. In this case, the absence of pancreatitis and the patient’s juvenile age suggest a distinct etiopathogenesis—possibly local ischemia or congenital ductal vulnerability exacerbated by the metabolic stress of diabetes.
The coexistence of juvenile DM and pancreatic infection presents a diagnostic paradox: was insulin deficiency secondary to pancreatic damage, or did hyperglycemia predispose to infection? Regardless of sequence, both pathologies mutually aggravate systemic inflammation and metabolic instability.
Therapeutic approach: conservative yet effective
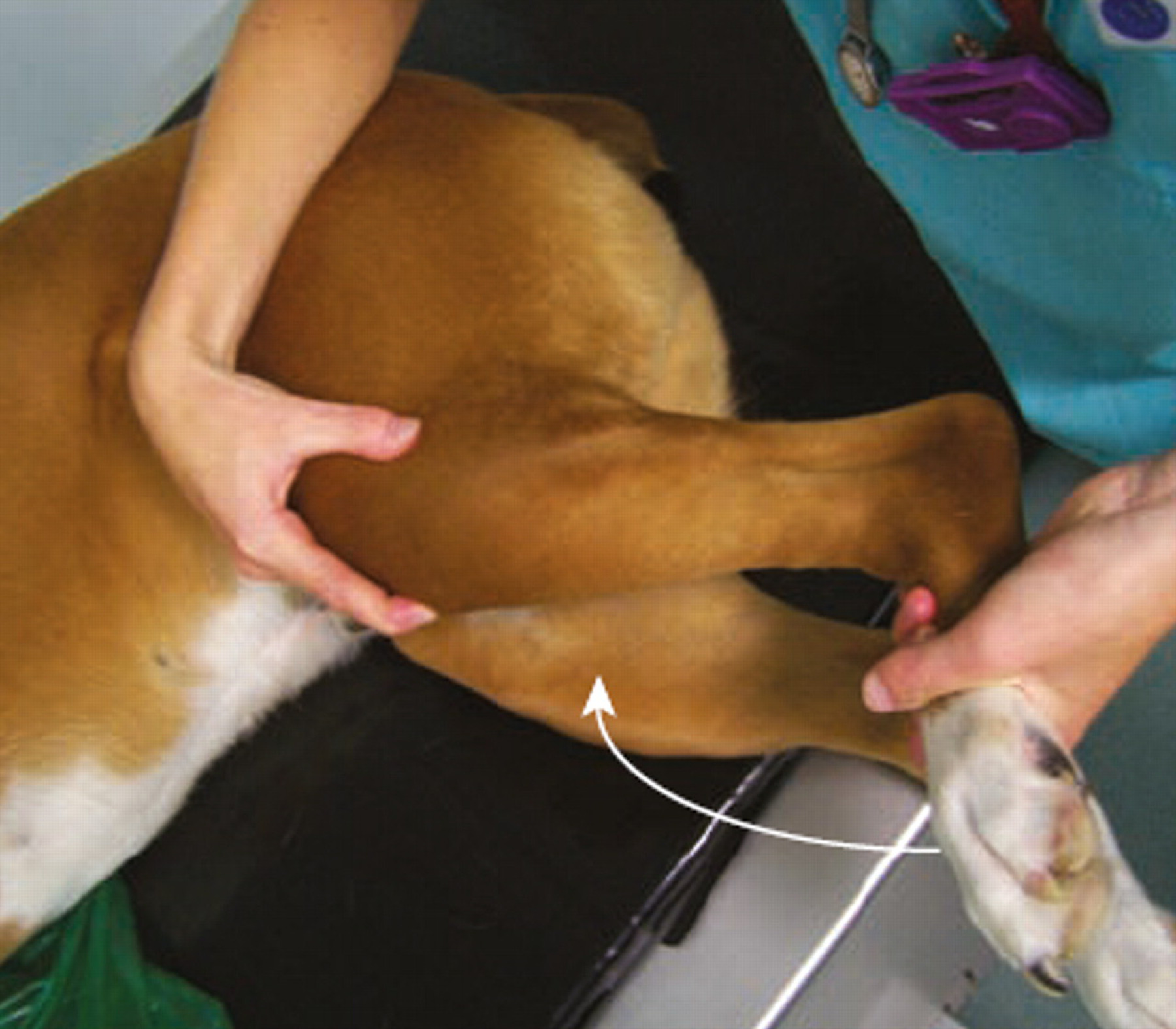
Given the high anesthetic and surgical risk in a juvenile, ketotic diabetic, the clinicians opted for a minimally invasive strategy—ultrasound-guided percutaneous drainage combined with medical therapy1.
- Under ultrasound guidance, a fine-needle aspiration yielded ~2 mL of purulent material.
- The abscess cavity was drained; cytology confirmed pyogranulomatous inflammation.
- Broad-spectrum antibiotics were initiated empirically for two weeks.
- Porcine lente insulin (1.5 U/kg SC q12 h) was started with close glucose monitoring.
- Supportive care (fluids, electrolytes, nutrition) was maintained.
Follow-up ultrasounds on days 7, 14, 21 and at 5 months confirmed complete resolution with no recurrence. Remarkably, at 1-year follow-up, the dog maintained stable glycemic control.
Context from broader literature
Historically, pancreatic abscesses in dogs were treated surgically, often with high mortality rates ranging from 33 % to 86 %. However, recent data support medical and minimally invasive approaches.
A retrospective study by Talbot et al. (2022) evaluated 15 canine cases with pancreatic fluid accumulations and found that medical or combined (medical + drainage) management achieved survival in most dogs, with several recovering without surgical intervention2.
Together, the findings of Daravigka et al. and Talbot et al. reinforce a paradigm shift: not all pancreatic abscesses mandate immediate surgery. Selected patients—especially those with concurrent systemic disease such as diabetes mellitus—may benefit from a stepwise, conservative protocol guided by ultrasound and close monitoring.
Key take-home messages for clinicians
- Suspect pancreatic pathology in diabetic dogs showing vomiting, anorexia, or disproportionate inflammation. Even in young animals, abscessation is possible.
- Ultrasound is indispensable for detecting pancreatic fluid lesions and guiding minimally invasive interventions.
- Medical management can succeed: drainage plus antibiotics and metabolic stabilization may suffice, especially when surgery poses excessive risk.
- Coordinate diabetic control: concurrent insulin therapy and metabolic correction are vital for resolution and long-term stability.
- Monitor dynamically: serial ultrasonography ensures lesion regression and early detection of recurrence.
- Reassess surgical need: Reserve exploratory surgery for non-resolving or recurrent abscesses, in line with current evidence.
Practical recommendations
- Perform full biochemical work-ups including fructosamine, HbA1c, and β-hydroxybutyrate in suspected DM cases.
- Utilize cPL and cTLI assays to differentiate between pancreatitis, abscess, and exocrine insufficiency.
- In fluid collections, prioritize ultrasound-guided aspiration for cytology and culture before considering open surgery.
- Manage glycemia aggressively; early insulin therapy supports immune and metabolic recovery.
- Provide owners with clear home-monitoring instructions and schedule structured follow-ups.
Conclusion
The case by Daravigka et al. (2025) underscores that even complex presentations—juvenile diabetes with pancreatic abscess—can be successfully managed conservatively when guided by imaging and careful medical oversight. When viewed alongside the broader experience summarized by Talbot et al. (2022), it becomes evident that ultrasound-guided drainage and medical therapy represent viable, often preferable options for selected canine patients.
As the veterinary community refines its approach to pancreatic diseases in dogs, combining metabolic control, interventional imaging, and evidence-based decision-making will remain key to improving survival and quality of life in diabetic patients.
References
- Daravigka A, Ninis S, Bourdekas P, Konstantinidis A.O., Ginoudis A, Adamama-Moraitou K.K., Lyraki M., Soubasis N. Successful Management of a Pancreatic Abscess in a Dog with Juvenile Diabetes Mellitus Through Ultrasound-Guided Drainage and Medical Therapy. Vet Sci. 2025; 12(7):604.
- Talbot C.T., Cheung R., Holmes E.J., Cook S.D. Medical and Surgical Management of Pancreatic Fluid Accumulations in Dogs: A Retrospective Study of 15 Cases. J Vet Intern Med. 2022; 36:919–926.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...