
Article
Unraveling MUO in Dogs: From Breed Susceptibility to Immune-Mediated Pathways
Among canine neurological conditions, Meningoencephalitis of Unknown Origin (MUO) remains one of the most challenging to diagnose and manage. Once considered a vague, catch-all term for non-infectious encephalitis, MUO is now recognized as a spectrum of immune-mediated inflammatory diseases of the central nervous system (CNS), including Granulomatous Meningoencephalomyelitis (GME) and Necrotizing Encephalitides (NME/NLE)1.
Although the exact cause is unclear, increasing evidence supports an autoimmune origin, where the dog’s own immune system attacks the brain and spinal cord.
What Exactly is MUO?
MUO refers to a presumed immune-mediated inflammation of the brain, sometimes extending to the spinal cord.
Dogs commonly present with seizures, ataxia, circling, blindness, cranial nerve deficits, or behavioural changes, depending on the lesion’s location1.
It remains a diagnosis of exclusion, made only after infectious causes have been ruled out using serology, CSF analysis, or PCR testing2.
Clinical Tip: When a small-breed dog under six years presents with acute neurological signs and no fever, MUO should be considered an important differential3,4.
Histopathologically, MUO is characterized by mononuclear infiltrates, perivascular cuffing, and areas of necrosis, especially in necrotizing variants5.
Inside the Immune Storm
MUO is now viewed as an autoimmune CNS disease driven by abnormal T-cell activity. Studies indicate that Th17 cells and cytokines such as IL-17 and IFN-γ play a major role in driving inflammation and neuronal damage6.
Lesions show lymphocytic and macrophagic infiltration with demyelination, often resembling multiple sclerosis in humans7.
MRI typically shows multifocal, asymmetric T2/FLAIR hyperintensities, while CSF findings reveal lymphocytic pleocytosis and elevated protein8.
Clinical Note: MRI combined with CSF analysis remains the most reliable method for early MUO detection3.
MUO vs. Infectious Encephalitis — Quick Comparison
Both MUO and infectious encephalitis can present similarly. Differentiating them early helps guide correct treatment9.
MUO — Key Features
- No systemic fever
- Signs vary with lesion site
- Common findings: Altered mentation, cranial nerve and proprioceptive deficits, ataxia, seizures
- CSF: Lymphocytic pleocytosis
- MRI: Multifocal lesions
- Infectious testing: Negative
Infectious Encephalitis — Key Features
- May have fever
- Overlapping neurological signs (ataxia, seizures, cranial nerve deficits)
- CSF: Neutrophilic or mixed response
- PCR or serology: May be positive
- Possible exposure history — tick bites, travel, or local outbreaks
Clinical Reminder: Always rule out infectious causes before initiating corticosteroids. Early immunosuppression may mask infection and complicate diagnosis.
Breed Predispositions & Genetic Factors
Certain small and toy breeds show consistent patterns of MUO, suggesting a heritable immune predisposition.
- In Pugs, necrotizing meningoencephalitis (NME) has a strong association with DLA/MHC class II haplotypes (DRB1-010011, DQA1-00201, DQB1-01501), supporting an autoimmune genetic link3,11.
- Maltese and Chihuahuas also exhibit MHC II–linked risks, indicating a shared immune mechanism3.
- GME is less clearly linked to genetics but may involve similar autoimmune pathways in predisposed small breeds.
Table 1. MUO Subtypes, Histopathology, and Breed Predispositions3,10
|
Subtype |
Key Histopathology |
Common CNS Localization |
Breed/Age Predisposition |
Genetic/Immune Associations |
Notes |
|
GME (Granulomatous Meningoencephalomyelitis) |
Angiocentric or nodular granulomatous inflammation with macrophage-rich cuffs |
Cerebellum, brainstem, spinal cord |
Middle-aged small breeds (Terriers, Poodles) |
T-cell–mediated; autoimmune pathways suspected |
May overlap with necrotizing variants |
|
NME (Necrotizing Meningoencephalitis) |
Necrosis in cortex/meninges; non-suppurative inflammation |
Cerebrum and meninges (gray matter) |
Young Pugs, Maltese |
Linked to MHC II haplotype (DRB1-010011, DQA1-00201, DQB1-01501); ↑ anti-GFAP antibodies |
Autoimmune predisposition; early onset |
|
NLE (Necrotizing Leukoencephalitis) |
White matter necrosis; lymphocytic perivascular infiltration |
Subcortical white matter, brainstem |
Yorkshire Terriers, Chihuahuas |
Possible MHC II link; under study |
Often overlaps with NME |
|
Other MUO Variants |
Lympho-histiocytic or vasculitic inflammation |
Variable |
Greyhounds, Australian Shepherds (senior onset) |
Not defined |
May represent other autoimmune subtypes |
Clinical Insight:
- Young toy breeds → often necrotizing forms (NME/NLE) with genetic-immune basis.
- Middle-aged small breeds → commonly GME, an immune-mediated variant.
Reflective Insight
MUO is no longer the vague “mystery inflammation” it was once thought to be. It represents a complex but decipherable immune disorder that rewards early recognition and evidence-based interpretation. Understanding its genetic and immunologic framework helps clinicians approach each case with greater confidence and helps patients achieve a better long-term outcome.
References
- Cornelis I, Van Ham L, Gielen I, De Decker S, Bhatti SF. Clinical presentation, diagnostic findings, prognostic factors, treatment and outcome in dogs with meningoencephalomyelitis of unknown origin: a review. The Veterinary Journal. 2019 Feb 1;244:37-44.
- Bach FS, Cray C, Burgos AP, Junior JA, Montiani-Ferreira F. A comparison between neurological clinical signs, cerebrospinal fluid analysis, cross-sectional CNS imaging, and infectious disease testing in 168 dogs with infectious or immune-mediated meningoencephalomyelitis from Brazil. Frontiers in veterinary science. 2023 Oct 25;10:1239106.
- Nessler JN, Tipold A. Of potential new treatment targets and polythetic approach in meningoencephalitis of unknown origin: a review. Frontiers in veterinary science. 2024 Oct 15;11:1465689.
- Barber R, Downey Koos L. Treatment with cytarabine at initiation of therapy with cyclosporine and glucocorticoids for dogs with meningoencephalomyelitis of unknown origin is not associated with improved outcomes. Frontiers in Veterinary Science. 2022 Jun 10;9:925774.
- Robinson KE. Transcriptomic evaluation of granulomatous and nectrotizing meningoencephalitis of dogs. University of Georgia, Athens, Georgia. 2020:80.
- Barber R, Barber J. Differential T-cell responses in dogs with meningoencephalomyelitis of unknown origin compared to healthy controls. Frontiers in Veterinary Science. 2022 Aug 4;9:925770.
- Zdora I, Raue J, Söbbeler F, Tipold A, Baumgärtner W, Nessler JN. Case report: Lympho-histiocytic meningoencephalitis with central nervous system vasculitis of unknown origin in three dogs. Frontiers in veterinary science. 2022 Aug 24;9:944867.
- Levitin HA, Lampe R, Hecht S. Case report: meningoencephalomyelitis of unknown etiology manifesting as a bilateral cranial polyneuropathy in 3 dogs. Frontiers in Veterinary Science. 2020 Jun 12;7:326.
- Patterson A. Meningoencephalomyelitis of Unknown Origin in Dogs. Vet Ir J Small Animal. 2023 Nov; (Small Animal Continuing Education)
- Oshima A, Ito D, Katakura F, Miyamae J, Okano M, Nakazawa M, Kanazono S, Moritomo T, Kitagawa M. Dog leukocyte antigen class II alleles and haplotypes associated with meningoencephalomyelitis of unknown origin in Chihuahuas. Journal of Veterinary Medical Science. 2023;85(1):62-70.
Related Experts
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
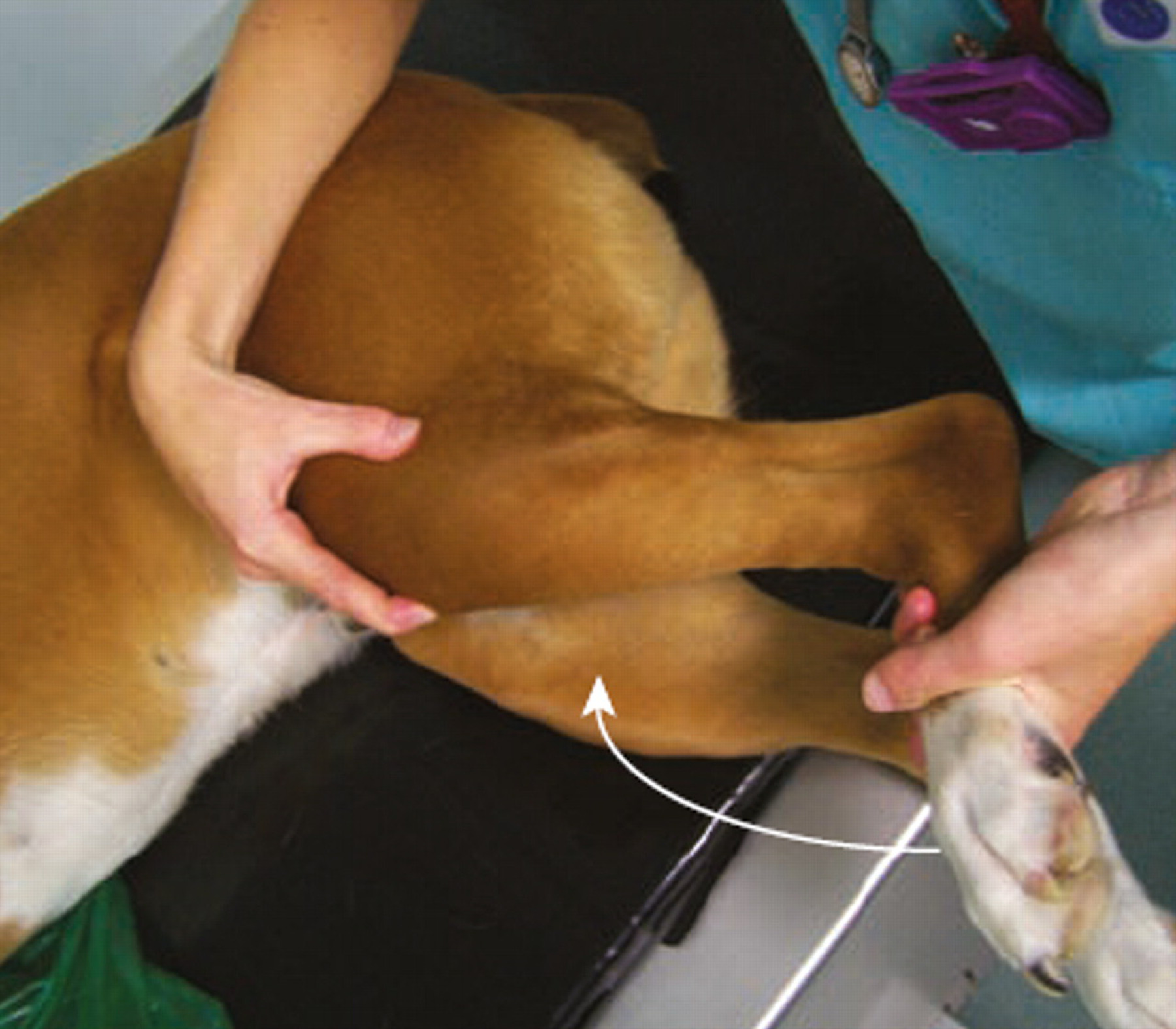
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...
