
Article
Top 5 Pitfalls in Feline Femoral Fracture Management
Feline femoral fractures are among the most challenging orthopedic injuries in small animal practices. Successful management demands an understanding of:
- Feline bone morphology,
- Mechanical load distribution, and
- Soft-tissue considerations.
Precise diagnosis, meticulous preoperative planning, and gentle surgical execution are vital to minimize complications and optimize recovery. Even experienced veterinarians can encounter difficulties if critical principles are overlooked. Recognizing and avoiding common pitfalls improves healing, long-term limb function, and patient outcomes.
1. Overlooking Physeal Preservation in Juvenile Cats
Common Mistake: Using rigid implants that cross the physis or applying excessively stiff fixation in growing cats.
Why It Matters: Disruption of the growth plate can lead to angular deformities, limb shortening, and permanent gait abnormalities2.
Evidence: Rubinos and Meeson reviewed 36 juvenile feline femoral fractures and found that physeal-sparing fixation—using smooth K-wires or cross-pins—achieved normal limb alignment in over 85% of cases. Roberts and Meeson recommend reserving plating for unstable or severely displaced juvenile fractures1.
Vet Insights:
- Identify the physis clearly on preoperative and intraoperative imaging.
- Avoid screws or plates crossing the physis whenever possible.
- For simple, nondisplaced fractures, use minimally invasive fixation to preserve remaining growth potential.
- Reevaluate alignment and limb length during radiographic follow-up at 4–6 weeks postoperatively.
2. Selecting Inadequate Fixation for Diaphyseal Fractures
Common Mistake:
Relying on intramedullary (IM) pins alone for femoral diaphyseal fractures that must withstand bending, axial, and torsional loads.
Why It Matters:
IM pins primarily resist bending but provide poor torsional and axial stability, making them unsuitable as stand-alone fixation for most diaphyseal fractures. This increases the risk of instability, delayed union, malunion, or postoperative mechanical complications¹,⁴.
Evidence:
Roberts & Meeson clearly state that IM pins should not be used as the sole fixation for diaphyseal femoral fractures because they do not counteract rotational or compressive forces. Instead, they recommend bone plates or plate-rod constructs, which provide multidirectional stability1.
Zurita & Craig reinforce this by noting that bone plates, external skeletal fixators, plate-rod constructs, and interlocking nails can all achieve successful healing when applied appropriately, whereas IM pins alone are biomechanically insufficient for diaphyseal fractures. They also emphasise that fracture complexity, patient weight, and soft-tissue injury significantly influence fixation choice and healing outcomes3.
Vet Insights:
- Evaluate fracture geometry, soft-tissue injury, and expected load before choosing fixation.
- For unstable, comminuted, or high-energy fractures, choose constructs with strong rotational and axial stability (locking plates, plate-rod constructs, or interlocking nails).
- Use orthogonal radiographs or fluoroscopy intraoperatively to verify alignment, implant placement, and construct stability.
3. Mismanaging Distal and Proximal Femoral Fractures
Common Mistake: Using simple fixation methods such as cross-pins for complex distal or proximal femoral fractures without accounting for instability or muscular tension.
Why It Matters: Inadequate fixation strength or failure to address quadriceps tension can lead to loss of reduction, malalignment, or delayed healing⁴⁻⁶. Proximal fractures often occur alongside other orthopaedic or pelvic injuries, requiring coordinated planning⁷.
Evidence: Yayla et al.⁴ found that cross-pinning is effective for simple supracondylar fractures, whereas complex or unstable distal fractures benefit from more robust fixation, including hybrid ESF.
Gülaydın and Alkan⁵ demonstrated that hybrid ESF provides strong stabilisation and good outcomes for distal comminuted fractures, supporting its use in challenging configurations.
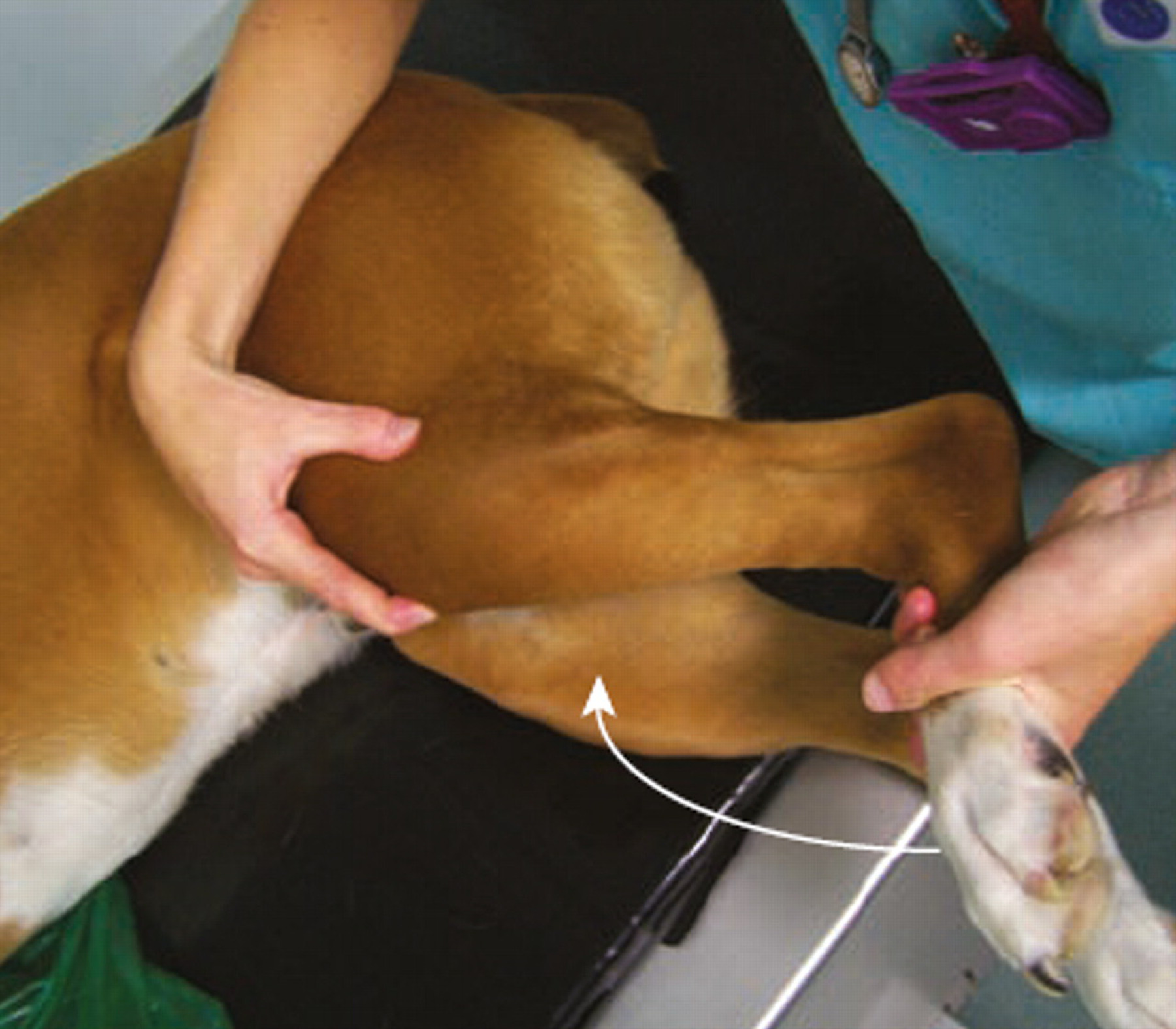
For proximal femoral fractures, Rustemeyer and Schmierer⁶ reported that complete vastus release reduces quadriceps tension, facilitating anatomic reduction and improving surgical access.
Nurra et al.⁷ highlighted that greater trochanteric fractures frequently present with concurrent pelvic or femoral injuries, underscoring the need for comprehensive trauma evaluation.
Vet Insights:
- Use hybrid ESF for unstable, supracondylar, or comminuted distal femoral fractures.
- Consider a vastus lateralis release for difficult proximal fractures to overcome quadriceps tension.
- Evaluate for concurrent pelvic or femoral injuries in all proximal fracture cases.
- Plan pin and screw placement carefully to avoid joint penetration and preserve muscle function.
4. Neglecting Soft-Tissue Care and Postoperative Rehabilitation
Common Mistake: Rough soft-tissue manipulation, excessive periosteal stripping, or delaying the start of rehabilitation.
Why It Matters: Poor soft-tissue handling and delayed mobilisation increase the risk of fibrosis, quadriceps contracture and joint stiffness, and can delay functional recovery¹,³.
Evidence: Roberts & Meeson state that delays to repair and extensive soft-tissue injury increase the risk of quadriceps contracture and emphasise careful tissue handling and appropriately timed postoperative mobilisation.¹ Zurita & Craig highlight that soft-tissue damage and contamination influence fixation choice (for example, favouring ESF in contaminated wounds) and that follow-up and rehabilitation timing should be tailored to fracture complexity and patient factors.³
Vet Insights:
- Minimise soft-tissue trauma and preserve the muscle envelope during exposure and implant placement.
- Begin controlled physiotherapy and gradual weight-bearing once fixation is stable and wound healing permits.
- Provide multimodal analgesia and instruct owners on pin-site care (for ESF) and on stepwise activity progression to avoid adhesions and stiffness.
5. Failing to Identify Concurrent Injuries
Common Mistake: Focusing solely on the femoral fracture without screening for additional trauma.
Why It Matters:
High-energy mechanisms frequently produce multiple injuries—including pelvic damage or contralateral limb fractures—which dramatically influence weight-bearing, rehabilitation planning, and overall prognosis.⁷
Evidence:
Nurra et al.⁷ reported a high prevalence of concurrent injuries in cats with femoral fractures, with pelvic fractures and additional long-bone injuries being particularly common. Missing these associated injuries complicates postoperative management and may worsen outcomes.
Vet Insights:
- Perform full-body imaging (radiography or CT) when high-energy trauma is suspected.
- Assess for neurological deficits, pelvic instability, and soft-tissue damage.
- Prioritize systemic or life-threatening injuries before orthopaedic repair to optimize survival and long-term function.
Conclusion
Effective management of feline femoral fractures relies on preserving growth potential in juveniles, applying fixation appropriate to fracture mechanics, and prioritizing soft-tissue integrity. Comprehensive preoperative evaluation, precise surgical technique, and early postoperative rehabilitation are crucial to maximize functional outcomes. Integrating these evidence-based principles across all stages of care minimizes complications and supports optimal recovery in feline patients (1–7).
References
- Roberts VJ, Meeson RL. Feline femoral fracture fixation: what are the options? J Feline Med Surg. 2022;24(5):442–63. Available from: https://journals.sagepub.com/doi/full/10.1177/1098612X221090391
- Rubinos C, Meeson RL. Traumatic physeal fractures in cats: a review of 36 cases (2010–2020). J Feline Med Surg. 2022;24(2):98–106.
- Zurita M, Craig A. Feline diaphyseal fractures: management and treatment options. J Feline Med Surg. 2022;24(7):662–74.
- Yayla S, Altan S, Çatalkaya E, Kanay BE, Saylak N. Evaluation of supracondylar femur fractures in cats: a retrospective study. Iran J Vet Sci Technol. 2022;14(4):37–41.
- Gülaydın A, Alkan İ. Evaluation of distal femur fractures in cats by hybrid external fixator. Ankara Univ Vet Fak Derg. 2024;71(1):89–100.
- Rustemeyer L, Schmierer PA. Complete vastus release to repair complex proximal femoral fractures: description and follow-up in four cats. J Feline Med Surg. 2025;27(9):1098612X251367614.
- Nurra G, Pilot M, Grek-Fritzner B, Coppola M, Grierson JM, Langley-Hobbs S. Fracture of the greater trochanter of the femur in 17 cats: imaging, clinical features and concurrent injuries. J Feline Med Surg. 2025;27(4):1098612X241305918.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
Article
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...