.jpg)
Article
Feline Lower Urinary Tract Diseases: 2025 iCatCare Clinical Algorithm
Lower urinary tract signs (LUTS) in cats—including dysuria, haematuria, periuria, pollakiuria, and stranguria are common presenting complaints1. Multiple conditions can cause these signs, including feline idiopathic cystitis (FIC), urolithiasis, urinary tract infections, neoplasia, and anatomical abnormalities. Because of this overlap, a structured, algorithm-based diagnostic approach is critical to ensure accurate diagnosis, avoid unnecessary interventions, and optimize patient outcomes.
Why a Structured Algorithm Matters
- LUTS etiology can vary between episodes, even in the same patient.
- Assuming recurrence indicates the same disease is a common pitfall.
- Investigations should be tailored based on:
- Severity of clinical signs
- Patient history and recurrence pattern
- Caregiver resources
Goal: Improve diagnostic accuracy, reduce antibiotic misuse, and enhance communication with caregivers.
Step 1 – Decoding History2
A thorough history is the cornerstone of LUTS diagnosis.
1.1 Clinical Signs
- Record type, frequency, and duration of LUTS.
- Include systemic signs such as vomiting, inappetence, or lethargy.
1.2 Environmental & Behavioral Factors
- Stressors: new pets, visitors, or environmental changes
- Litter box hygiene and preferences
- Outdoor access and indirect urination clues (perineal staining, hair loss, abnormal indoor urination)
2.3 Caregiver Observations
- Urine volume, color, and frequency
- Estimate urine volume via litter clumps for clumping litter
Tip: Use structured caregiver questionnaires to gather complete and consistent information.
Step 2 – Physical Examination2
Provides context and clues even if it rarely confirms LUT disease.
2.1 General Assessment
- Vital signs, body weight, body condition, and muscle scores
- Hydration assessment, particularly in urethral obstruction cases
2.2 Abdominal & Perineal Exam
- Bladder palpation:
- Firm, distended, painful → likely urethral obstruction (emergency)
- Small, thickened → chronic LUTD
- Kidneys: check for asymmetry or pain
- Perineum: look for self-trauma or gritty material
Step 3 – Laboratory Testing2
3.1 Serum Biochemistry
- Common findings: azotaemia, hyperkalaemia, hypocalcaemia, hypoalbuminaemia
- Variable hyponatraemia, hyperphosphataemia, hyperglycaemia106,109
- Serum symmetric dimethylarginine (SDMA) may be elevated (>20 μg/dl)110
3.2 Electrocardiography
- Recommended even without bradycardia
- Hyperkalaemia ECG changes: prolonged PR, absent/reduced P waves, widened QRS, shortened QT, tall/tented/reversed T waves
- Severe hyperkalaemia: sinoventricular rhythm, atrial standstill, ventricular fibrillation, asystole
- ECG findings approximate potassium concentration; discordance may occur109
Stabilize urethral obstruction before any further testing.
Step 4 – Urinalysis2
Urinalysis is essential and must be precise.
4.1 Sample Collection
- Preferred: cystocentesis before antibiotics
- Avoid: manual bladder expression or catheterization for culture
- Alternative: clean non-absorbent litter for difficult cats
4.2 Key Measurements2
- Specific gravity: <1.035 → consider systemic disease
- Sediment: examine within 1 hour to prevent artefacts
- Protein: use urine protein:creatinine ratio
- pH: repeat measurements recommended
4.3 Special Considerations
- Alpha-2 agonists can falsely lower USG
- Crystalluria may be artefactual
- Lipiduria is normal in cats
Tip: Follow 2022 AAFP/ISFM Cat Friendly Veterinary Interaction Guidelines to minimize stress during cystocentesis.
Step 5 – Imaging
Indicated for recurrent, severe, or atypical LUTS.
5.1 Abdominal Radiography2
- Detect radiodense uroliths, urethral strictures, bladder distension
- Lateral & dorsoventral views including pelvic & penile urethra
- Enema improves visualization
- Radiography identifies underlying cause in 30–40% of UO cases
- Avoid confusing os penis with distal urethral stones
5.2 Ultrasonography2,4
- Detect calculi, masses, clots, debris, congenital abnormalities
- Assess kidneys, ureters, abdominal organs
- Limitation: intrapelvic and penile urethra visualization
5.3 Retrograde Urethrography2
Indications: inconclusive ultrasound or suspected urethral pathology
Key Steps:
- Plain radiography first
- Moderate bladder distension
- Evacuate feces or perform enema
- Sterile catheter placement
- Slow contrast injection (150–200 mg iodine/ml, 1 ml/kg)
- Radiographs during last stage of injection
Use: Evaluate patency, strictures, ruptures, or filling defects.
5.4 Advanced Imaging
- CT: Identify congenital or anatomical abnormalities
- MRI: Rare, for neurological LUTS (incontinence, retention)
5.5 Cystourethroscopy
- Visualize masses, uroliths, glomerulations
- Facilitate biopsy or minimally invasive removal
- Limited by small feline size
5.6 Point-of-Care Ultrasound (POCUS) for Urethral Obstruction2
- Use for rapid assessment of fluid status and early detection of overload in cats with urethral obstruction.
- Monitor parameters: left atrial-to-aortic ratio, CVC diameter, left ventricular size and wall thickness, cavitary effusion, B-lines in the lung, gallbladder edema.
- CVC assessment: collapsed in volume depletion, distended in overload; healthy cats show ≥20% change with respiration.
- Serial monitoring can guide fluid therapy and detect evolving overload.
- Can also examine the bladder for fluid; presence of fluid does not rule out tear/leak.
Step 6 – Diagnostic Roadmap
Follow a logical, sequential approach:
- History →Physical Examination →Urinalysis & Laboratory Tests →Imaging (Radiography + Ultrasound) →Advanced Imaging / Cystourethroscopy if needed →Interpretation & Action
Clinical Examples:
- Haematuria, no bacteria/crystals → likely FIC → focus on environmental modification and analgesia.
- Struvite crystals, alkaline urine → urolithiasis → dietary or surgical management.
- Positive urine culture → infection → appropriate antibiotic therapy.
Key Takeaways
- Recurrent LUTS may have different causes; never assume same etiology.
- Urinalysis is critical—interpret results cautiously.
- Imaging complements urinalysis, especially for complex cases.
- Retrograde urethrography and advanced imaging are for selected cases.
- Always rule out urethral obstruction first—a medical emergency.
Conclusion
A structured, stepwise approach using the 2025 iCatCare algorithm allows veterinarians to efficiently evaluate and manage cats with LUTS. By integrating history, physical examination, urinalysis, and appropriate imaging, clinicians can make accurate diagnoses, avoid unnecessary interventions, and improve patient outcomes.
References
- Dorsch R, Teichmann-Knorrn S, Sjetne Lund H. Urinary tract infection and subclinical bacteriuria in cats: a clinical update. Journal of feline medicine and surgery. 2019 Nov;21(11):1023-38.
- Taylor S, Boysen S, Buffington T, Chalhoub S, Defauw P, Delgado MM, Gunn-Moore D, Korman R.
2025 iCatCare consensus guidelines on the diagnosis and management of lower urinary tract diseases in cats.
J Feline Med Surg. 2025 Feb; 27(2): 1098612X241309176. © SAGE Publications.
- Pollard RE, Phillips KL. Diagnostic imaging of the urinary tract. In: Elliott J, Grauer GF, Westropp JL (eds). BSAVA manual of canine and feline nephrology and urology. Quedgeley, UK: BSAVA, 2017, pp 84-115.
- Griffin S. Feline abdominal ultrasonography: what's normal? What's abnormal? Renal pelvis, ureters and urinary bladder. J Feline Med Surg 2020; 22: 847-865.
Related Contents
.jpg)
Article
Immunoprophylaxis and Vaccines for Lumpy Skin Disease in India
Lumpy Skin Disease (LSD) is a capripoxvirus-induced viral disease affecting cattle and buffaloe...
.jpg)
Article
Lumpy Skin Disease in India: Diagnostic Challenges, Differential Diagnoses, and Laboratory Confirmation
Lumpy Skin Disease (LSD) is a contagious viral disease of cattle caused by Lumpy Skin Disease Virus...

Article
Lumpy Skin Disease: From Clinical Signs to Field-Level Control
Lumpy Skin Disease (LSD) is a highly contagious viral disease of cattle and buffaloes caused by the...

Article
Antimicrobial Resistance: Breaking Professional Silos to Protect the Future of Medicine
Antimicrobial resistance (AMR) has evolved into a critical global health problem affecting humans, a...

Article
Environmental Health, Animal Health, Human Health – Connecting the Missing Links
The health of humans, animals, and the environment is increasingly understood to be i...

Article
Zoonotic Diseases Without Borders: Why One Health Collaboration Starts with Veterinarians
Zoonotic diseases, those that are transmitted between animals and humans, represent some of the grea...

Article
From Clinics to Communities – The Veterinarian’s Expanding Role in One Health
In the evolving landscape of global health, veterinarians are no longer confined to treating&nb...
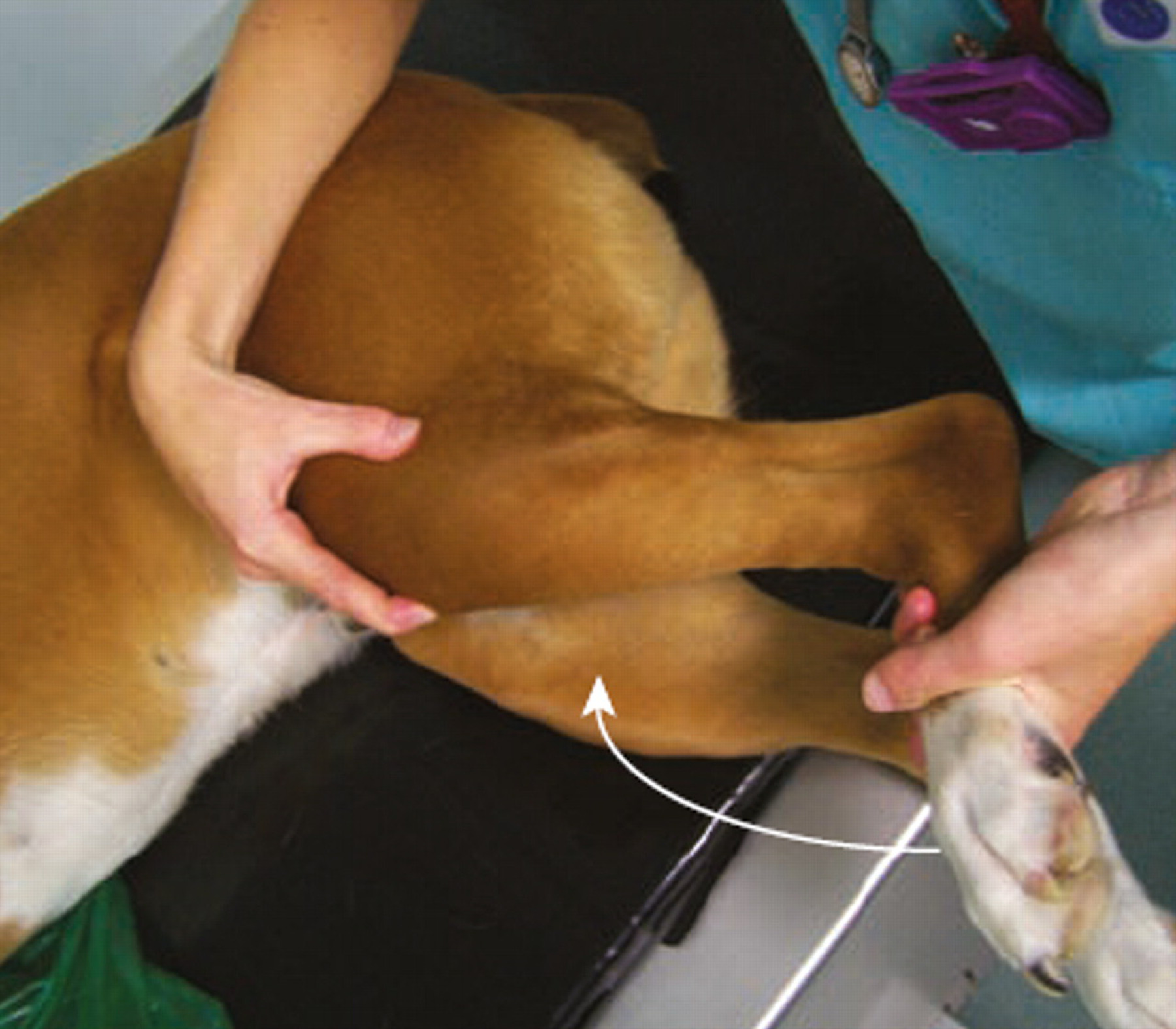
Article
Meniscal Tears in Dogs With Cranial Cruciate Ligament Rupture: Clinical Implications for Practitioners
Introduction Cranial cruciate ligament (CCL) rupture is a leading cause of stifle in...